Abstract
Introduction and hypothesis
Pelvic floor muscle training (PFMT) is internationally recommended for prevention and treatment of urinary incontinence (UI) and pelvic organ prolapse (POP). However, there is lack of knowledge about PFMT among pregnant Nepalese women. The objectives of this study were to develop a PFMT programme and to assess the feasibility of the programme.
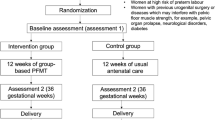
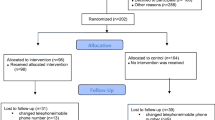
Methods
A feasibility study was conducted to address aspects of the PFMT programme provided to pregnant women attending antenatal check-ups at Kathmandu University Dhulikhel Hospital. The women were recruited consecutively from June 2017 to April 2018. The PFMT programme consisted of attending a minimum of four supervised PFMT follow-up visits after inclusion to the programme and performing PFMT daily at home. Feasibility was assessed in terms of the recruitment capability, sample characteristics, data collection procedures, outcome measures, and acceptability (attendance to PFMT visits, PFMT adherence, participant experiences) of the programme. Data were collected using self-reported questionnaires. Educational material (video, leaflet, and exercise diary) was developed in Nepali.
Results
Among 253 women included, 144 (57%) attended four or more supervised PFMT visits. No significant differences were found in the symptoms of UI (0.89) and POP (0.44) between those attending and those not attending four PFMT visits. Half of the women adhered to 50–100% of PFMT daily at home. The supervised PFMT and the educational material motivated the women to daily PFMT.
Conclusion
The PFMT programme was acceptable, at least to those living in the district of the study site. The results and experiences from the current study may guide implementation and future studies on the effectiveness of PFMT in Nepal.

Similar content being viewed by others
References
Paul Abrams LC, Wagg A, Wein A. Incontinence. Tokyo: 6th International Consultation on Incontinence; 2017.
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29(1):4–20.
Shrestha B, Onta S, Choulagai B, Poudyal A, Pahari DP, Uprety A, et al. Women’s experiences and health care-seeking practices in relation to uterine prolapse in a hill district of Nepal. BMC Womens Health. 2014;14(1):20.
Regmi M, Uprety D, Poonam M. Prevalence of urinary incontinence among gynecological admissions at tertiary care hospital in eastern Nepal. Health Renaissance. 2012;10(1):16–9.
Gurung G, Rana A, Amatya A, Bista KD, Joshi AB, Sayami J. Pelvic organ prolapse in rural Nepalese women of reproductive age groups: What makes it so common? Aust N Z J Obstet Gynaecol. 2007;2(2):35–41.
Bonetti TR, Erpelding A, Pathak LR. Listening to “felt needs”: investigating genital prolapse in western Nepal. Reproductive Health Matters. 2004;12(23):166–75.
Nepal Government. Annual Report. Department of Health Services 2016/2017. Accessed on 20 December 2018. https://dohs.gov.np.
Radl CM, Rajwar R, Aro AR. Uterine prolapse prevention in Eastern Nepal: the perspectives of women and health care professionals. Int J Women's Health. 2012;4:373.
Schaaf JM, Dongol A, van der Leeuw-Harmsen L. Follow-up of prolapse surgery in rural Nepal. Int Urogynecol J. 2008;19(6):851–5.
Hagen S, Stark D. Conservative prevention and management of pelvic organ prolapse in women. The Cochrane Database of Systematic Reviews. 2011;(12):Cd003882.
Mørkved S, Bø K. Effect of pelvic floor muscle training during pregnancy and after childbirth on prevention and treatment of urinary incontinence: a systematic review. Br J Sports Med. 2014;48(4):299–310.
Boyle R, Hay-Smith EJ, Cody JD, Morkved S. Pelvic floor muscle training for prevention and treatment of urinary and faecal incontinence in antenatal and postnatal women. The Cochrane Database of Systematic Reviews. 2012;10:Cd007471.
DeLancey JO, Morgan DM, Fenner DE, Kearney R, Guire K, Miller JM, et al. Comparison of levator ani muscle defects and function in women with and without pelvic organ prolapse. Obstet Gynecol. 2007;109(2 Pt 1):295–302.
Brækken IH, Majida M, Engh ME, Bø K. Morphological changes after pelvic floor muscle training measured by 3-dimensional ultrasonography: a randomized controlled trial. Obstet Gynecol. 2010;115(2, Part 1):317–24.
Brækken IH, Majida M, Engh ME, Bø K. Can pelvic floor muscle training reverse pelvic organ prolapse and reduce prolapse symptoms? An assessor-blinded, randomized, controlled trial. Am J Obstet Gynecol. 2010;203(2):170. e1–7.
Eldridge SM, Lancaster GA, Campbell MJ, Thabane L, Hopewell S, Coleman CL, et al. Defining feasibility and pilot studies in preparation for randomised controlled trials: development of a conceptual framework. PLoS One. 2016;11(3):e0150205.
Orsmond GI, Cohn ES. The distinctive features of a feasibility study: objectives and guiding questions. OTJR. 2015;35(3):169–77.
Tibaek S, Dehlendorff C. Do women with pelvic floor dysfunction referred by gynaecologists and urologists at hospitals complete a pelvic floor muscle training programme? A retrospective study, 1992-2008. Int Urogynecol J. 2013;24(8):1361–9.
Slade SC, Dionne CE, Underwood M, Buchbinder R. Consensus on exercise reporting template (CERT): explanation and elaboration statement. Br J Sports Med. 2016;50(23):1428–37.
Eberhard-Gran MEA, Samuelsen SO, Tambs K. A short matrixversion of the Edinburgh depression scale. Acta Psychiatr Scand. 2007;116(3):195–200.
Hagen S, Glazener C, Sinclair L, Stark D, Bugge C. Psychometric properties of the pelvic organ prolapse symptom score. BJOG. 2009;116(1):25–31.
Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn. 2004;23(4):322–30.
Shijagurumayum Acharya R, Tveter AT, Grotle M, Khadgi B, Koju R, Eberhard-Gran M, et al. Cross-cultural adaptation and validation of the Nepali version of the pelvic girdle questionnaire. J Manipulative Physiol Ther. Accepted for publication on 7th April 2019.
Paiva LL, Ferla L, Darski C, Catarino BM, Ramos JG. Pelvic floor muscle training in groups versus individual or home treatment of women with urinary incontinence: systematic review and meta-analysis. Int Urogynecol J. 2017;28(3):351–9.
Hay-Smith EJ, Herderschee R, Dumoulin C, Herbison GP. Comparisons of approaches to pelvic floor muscle training for urinary incontinence in women. The Cochrane Database of Systematic Reviews. 2011;(12):Cd009508.
Sherburn M, Murphy CA, Carroll S, Allen TJ, Galea MP. Investigation of transabdominal real-time ultrasound to visualise the muscles of the pelvic floor. The Australian Journal of Physiotherapy. 2005;51(3):167–70.
Caagbay DM, Black K, Dangal G, Raynes-Greenow C. Can a leaflet with brief verbal instruction teach Nepali women how to correctly contract their pelvic floor muscles? J Nepal Health Res Counc. 2017;15(2):105–9.
Muhammad J, Muhamad R, Nik Husain N, Daud N. Pelvic floor muscle exercise education and factors associated with implementation among antenatal women in hospital Universiti Sains Malaysia. Korean J Fam Med. 2019;40(1):45–52.
Dumoulin C, Hay-Smith J, Frawley H, McClurg D, Alewijnse D, Bo K, et al. 2014 consensus statement on improving pelvic floor muscle training adherence: International Continence Society 2011 State-of-the-Science Seminar. Neurourol Urodyn. 2015;34(7):600–5.
Caagbay D, Black K, Wattimena J, Raynes-Greenow C. Teaching pelvic floor muscle training to local health workers in rural Nepal. Int J Health Promot Educ. 2018;56(6):289–97.
Acknowledgements
The authors thank the Obstetrics and Gynaecology Department at Kathmandu University Dhulikhel Hospital, Nepal, for providing permission to conduct the study. We also thank the research assistants Ms. Jashmi Maharjan and Ms. Jesmina Maharjan for help with data collection as well as Gill Brook for valuable help with the language editing of the manuscript and the video text. Finally, the authors thank all the women who participated in the study.
Funding
The study is funded by the Norwegian State Educational Loan Fund through the Norwegian Quota Scheme, Norway, and by the Association for Support of Physiotherapy in Nepal, Switzerland.
Author information
Authors and Affiliations
Contributions
R Shijagurumayum Acharya: Project development, data collection, data analysis, manuscript writing.
A Therese Tveter: Data analysis, critical revision of the manuscript.
M Grotle: Project development, critical revision of the manuscript.
I Hoff Braekken: Project development, critical revision of the manuscript.
B Khadgi: Project development, data collection, critical revision of the manuscript.
B Stuge: Project development, data analysis, critical revision of the manuscript.
The study was presented at the 7th International Conference of the Society of Obstetric Fistula Surgeons (ISOFS), Kathmandu, Nepal, 5–8th December 2018, as a poster presentation.
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shijagurumayum Acharya, R., Tveter, A.T., Grotle, M. et al. Pelvic floor muscle training programme in pregnant Nepalese women—a feasibility study. Int Urogynecol J 31, 1609–1619 (2020). https://doi.org/10.1007/s00192-019-04053-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-04053-1