Abstract
Introduction and hypothesis
The objective was to compare surgical outcomes after prior hysterectomy versus concomitant hysterectomy with laparoscopic/robotic minimally invasive sacral colpopexy (MISC).
Methods
Using all MISC from 2009 to 2014, patient sociodemographic and surgical data were compared between MISC with prior versus concomitant hysterectomy. Operative time (skin incision to closure) was compared with linear regression. Logistic regression compared complications, a composite variable including ≥1 transfusion, infection, readmission, reoperation, bowel obstruction/ileus, conversion to laparotomy, bowel/bladder injury, or mesh complication. Logistic regression compared prolapse recurrence defined as retreatment (pessary/surgery) or postoperative POP-Q points ≥ 0.
Results
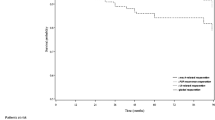
Eight hundred and sixteen patients were 59.6 ± 8.7 years old and predominantly Caucasians (97.8%), with BMI 27.4 ± 4.5 and predominantly POP-Q stage III prolapse (69.9%). Operative time was 205.0 ± 69.0 min. Concomitant hysterectomy increased operative time 17.8 min (p = 0.004) adjusting for age, POP-Q stage, total vaginal length, perineal body, lysis of adhesions or perineorrhaphy, changes in operating personnel (scrub tech/circulating nurse), case order during the day, and preoperative stress incontinence. Complications occurred in 15.8% and were more likely with prior hysterectomy (odds ratio [OR] = 2.30, 95% confidence interval [CI] = 1.43-3.70) adjusting for preoperative genital hiatus and perineal body, concomitant midurethral sling, obesity, and immunosuppression. During a follow-up of 31 weeks, 7.8% had prolapse recurrence with no impact from concomitant hysterectomy (OR = 0.96, 95% CI 0.41-2.24). Post-hoc power calculation would have required an unattainable size of >2,800 per group for this outcome.
Conclusions
For MISC, concomitant hysterectomy is associated with longer operative time but lower risk of complications. There was no impact of concomitant hysterectomy on prolapse recurrence, but longer follow-up may be needed for this outcome.
Similar content being viewed by others
References
FDA. Urogynecologic surgical mesh: update on the safety and effectiveness of transvaginal mesh placement for pelvic organ prolapse. US Food and Drug Administration; 2011. Accessed 20 March 2017.
Wu JM, Matthews CA, Conover MM, Pate V, Jonsson Funk M. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014;123:1201–6.
Nygaard I, Brubaker L, Zyczynski HM, Cundiff G, Richter H, Gantz M, et al. Long-term outcomes following abdominal sacrocolpopexy for pelvic organ prolapse. JAMA. 2013;309:2016–24.
Rosati M, Bramante S, Conti F. A review on the role of laparoscopic sacrocervicopexy. Curr Opin Obstet Gynecol. 2014;26:281–9.
Campbell P, Cloney L, Jha S. Abdominal versus laparoscopic Sacrocolpopexy: a systematic review and meta-analysis. Obstet Gynecol Surv. 2016;71:435–42.
O'Hanlan KA, Dibble SL, Garnier AC, Reuland ML. Total laparoscopic hysterectomy: technique and complications of 830 cases. JSLS. 2007;11:45–53.
Ismail SI, Emery SJ. Patient awareness and acceptability of antenatal perineal massage. J Obstet Gynecol. 2013;33:8.
Ismail SI. Recurrent prolapse after sacrocolpopexy for post-hysterectomy vaginal vault prolapse. J Obstet Gynecol. 2007;27:292–6.
Dallas K, Elliott CS, Syan R, Sohlberg E, Enemchukwu E, Rogo-Gupta L. Association between concomitant hysterectomy and repeat surgery for pelvic organ prolapse repair in a cohort of nearly 100,000 women. Obstet Gynecol. 2018;132:1328–36.
Geller EJ, Siddiqui NY, Wu JM, et al. Short-term outcomes of robotic sacrocolpopexy compared with abdominal sacrocolpopexy. Obstet Gynecol. 2008;112:1201–6.
Stepp KJ, Barber MD, Yoo EH, et al. Incidence of perioperative complications of urogynecologic surgery in elderly women. Am J Obstet Gynecol. 2005;192:1630–6.
Liss MA, Skarecky D, Morales B, et al. Preventing perioperative complications of robotic-assisted radical prostatectomy. Urology. 2013;81:319–23.
Turner LC, Kantartzis K, Lowder JL, Shepherd JP. The effect of age on complications in women undergoing minimally invasive sacral colpopexy. Int Urogynecol J. 2014;25:1251–6.
Barber MD, Brubaker L, Burgio KL, Richter HE, Nygaard I, Weidner AC, et al. Comparison of 2 transvaginal surgical approaches and perioperative behavioral therapy for apical vaginal prolapse: the OPTIMAL randomized trial. Eunice Kennedy Shriver National Institute of Child Health and Human Development Pelvic Floor Disorders Network. JAMA. 2014;12(311):1023–34.
Nager CW, Zyczynski H, Rogers RG, Barber MD, Richter HE, Visco AG, et al. The design of randomized trial of vaginal surgery for uterovaginal prolapse: vaginal hysterectomy with native tissue vault suspension versus mesh hysteropexy suspension (the study of uterine prolapse procedures randomized trial). Female Pelvic Med Reconstr Surg. 2016;22:182–9.
Giugale LE, Sears S, Lavelle ES, Carter-Brooks CM, Bonidie M, Shepherd JP. Evaluating the impact of intraoperative surgical team handoffs on patient outcomes. Female Pelvic Med Reconstr Surg. 2017;23:288–92.
Lavelle ES, Turner LC, Shepherd JP. Impact of case order on laparoscopic sacrocolpopexy: do surgeons need a warm-up? Female Pelvic Med Reconstr Surg. 2017;23:272–5.
Vandendriessche D, Sussfeld J, Giraudet G, Lucot JP, Behal H, Cosson M. Complications and reoperations after laparoscopic sacrocolpopexy with a mean follow-up of 4 years. Int Urogynecol J. 2017;28:231–9.
Richter HE, Albo ME, Zyczynski HM, Kenton K, Norton PA, Sirls LT, et al. Urinary incontinence treatment network. Retropubic versus transobturator midurethral slings for stress incontinence. N Engl J Med. 2010;362:2066–76.
Rogers RG, Nolen TL, Weidner AC, Richter HE, Jelovsek JE, Shepherd JP, et al. Surgical outcomes after apical repair for vault compared with uterovaginal prolapse. Obstet Gynecol. 2018;131:475–83.
Culligan PJ, Murphy M, Blackwell L, Hammons G, Graham C, Heit MH. Long-term success of abdominal sacral colpopexy using synthetic mesh. Am J Obstet Gynecol. 2002;187:1473–80.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dubinskaya, A., Hernandez-Aranda, D., Wakefield, D.B. et al. Comparing laparoscopic and robotic sacrocolpopexy surgical outcomes with prior versus concomitant hysterectomy. Int Urogynecol J 31, 401–407 (2020). https://doi.org/10.1007/s00192-019-04017-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-04017-5