Abstract
Introduction and hypothesis
Pelvic organ prolapse (POP) and lower urinary tract symptoms (LUTs), in addition to cervical incompetence, have a multifactorial etiology. Connective tissue disorders are common risk factors in both entities. The objective of this study was to compare long-term urinary and pelvic organ prolapse-related symptoms in patients who experienced cervical incompetence and those who did not.
Methods
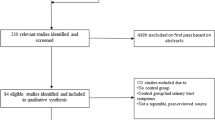
In this historical prospective cohort, analysis of cervical incompetence cases from one medical center between 2006 and 2009 were compared with a matched control group. All cases included a minimum 7-year follow-up. Symptoms of urinary and prolapse-related complaints during follow-up were evaluated based on the Pelvic Floor Distress Inventory-20 questionnaire.
Results
The study group comprised 37 women who experienced cervical incompetence matched to 34 consecutive controls. There was no difference between the groups in demographic or obstetric characteristics, except for a higher cesarean section rate and earlier deliveries among women with cervical incompetence. On assessment of patient’s symptoms, during follow-up, the average Pelvic Organ Prolapse Distress Inventory-6 score was significantly higher in patients who experienced cervical incompetence than in controls (15.0 ± 26.1 vs 1.7 ± 7.1 respectively, p = 0.034). Urinary complaints, as reflected by the Urinary Distress Inventory-6 index, were also more common in women with cervical incompetence (17.9 ± 19.1 vs 3.9 ± 7.3 p = 0.027).
Conclusions
Women with a history of cervical incompetence experienced a higher rate of pelvic organ prolapse and urinary symptoms compared with women who had no cervical insufficiency.
Similar content being viewed by others
References
Olsen AL, Smith VJ, Bergstrom JO, et al. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89:501–6.
Falconer C, Ekman G, Malmstrom A, et al. Decreased collagen synthesis in stress incontinent women. Obstet Gynecol. 1994;84:583–6.
Liu X, Zhao Y, Pawlyk B, et al. Failure of elastic fiber homeostasis leads to pelvic floor disorders. Am J Pathol. 2006;168:519–28.
ACOG Practice Bulletin. Cerclage for the management of cervical insufficiency. Obstet Gynecol. 2014;123(2 Pt 1):372–9.
Roman A, Suhag A, Berghella V. Overview of cervical insufficiency: diagnosis, etiologies, and risk factors. Clin Obstet Gynecol. 2016;59:237–40.
Rechberger T, Uldbjerg N, Oxlund H. Connective tissue changes during normal pregnancy and pregnancy complicated by cervical incompetence. Obstet Gynecol. 1988;71:563–7.
Petersen LK, Uldbjerg N. Cervical collagen in non-pregnant women with previous cervical incompetence. Eur J Obstet Gynecol Reprod Biol. 1996;67:41–5.
Schelmbach D, MacKay L, Shi L, et al. Cervical ripening and insufficiency: from biomechanical and molecular studies to in vivo clinical examination. Eur J Obstet Gynecol Reprod Biol. 2009;144:S70–6.
McIntosh LJ, Mallet VT, Frahm JD, et al. Gynecologic disorders in women with Ehlers Danlos syndrome. J Soc Gynecol Investig. 1995;2:559–64.
Carley ME, Schaffer J. Urinary incontinence and pelvic organ prolapse in women with Marfan or Ehlers Danlos syndrome. Am J Obstet Gynecol. 2000;182:1021–3.
Barber MD, Walters MD, Bump RC. Short forms of two condition specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol. 2005;193:103–13.
Tami L, Zuchelo S, Bezerra IMP, et al. Questionnaires to evaluate pelvic floor dysfunction in the postpartum period: a systematic review. Int J Women’s Health. 2018;10:409–24.
Sheyn D, Addae-Konaedu KL, Bauer AB, et al. History of cervical insufficiency increases the risk of pelvic organ prolapse and stress urinary incontinence in parous women. Maturitas. 2018;107:63–7.
Warren JE, Silver RM, Dalton J, et al. Collagen 1A1 and transforming growth factor-β polymorphisms in women with cervical insufficiency. Obstet Gynecol. 2007;110(3):619–23.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
There are no commercial associations that might create a conflict of interest in connection with the submitted manuscript. This applies to all the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ben-Zvi, M., Herman, H.G., Bar, J. et al. Are women with cervical incompetence at a higher risk of experiencing urinary and pelvic organ prolapse symptoms?. Int Urogynecol J 31, 385–389 (2020). https://doi.org/10.1007/s00192-019-03979-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-03979-w