Abstract
Introduction and hypothesis
There is conflicting evidence on whether intermittent catheterization (IC) is less associated with urinary tract infection (UTI) and more likely to prevent urinary retention than continuous catheterization (CC). We aimed to compare the effect of IC with that of CC on the incidence of postpartum UTI, urinary retention and hemorrhage in laboring women with epidural analgesia.
Methods
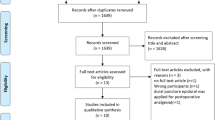
Electronic searches were performed in PubMed, EMBASE and Cochrane Library from their inception to October 2018. We selected RCTs comparing IC with CC in laboring women with epidural analgesia. A meta-analysis was performed using the RevMan software, and a random-effects model was used to pool the effect size. The Grades of Recommendation, Assessment, Development and Evaluation (GRADE) approach was used to rate the quality of evidence.
Results
Six RCTs (N = 850) were included in this review. The meta-analyses indicated that there was no significant difference between the IC and CC group in the incidence of postpartum UTI (RR = 1.25, 95% CI: 0.91 to 1.71, P = 0.16), postpartum urinary retention (RR = 0.76, 95% CI: 0.21 to 2.77, P = 0.68) and postpartum hemorrhage (RR = 1.72, 95% CI: 0.60 to 4.95, P = 0.31). GRADE assessment results showed that the quality of evidence was low.
Conclusions
Based on the available evidence, there is no measurable difference in rates of UTI between CC and IC, not that neither stragety decreases UTI, since the included trials do not address this.



Similar content being viewed by others
Abbreviations
- IC:
-
Intermittent catheterization
- CC:
-
Continuous catheterization
- UTI:
-
Urinary tract infection
- RCT:
-
Randomized clinical trial
- RR:
-
Risk ratio
- CI:
-
Confidence interval
- GRADE:
-
Grades of Recommendation, Assessment, Development and Evaluation
References
Ullman R, Smith LA, Burns E, et al. Parenteral opioids for maternal pain relief in labour. Cochrane Database Syst Rev. 2010;65(9):CD007396.
Traynor AJ, Aragon M, Ghosh D, et al. Obstetric anesthesia workforce survey: a 30-year update. Anesth Analg. 2016;122(6):1939.
Foon R, Toozs-Hobson P, Millns P, et al. The impact of anesthesia and mode of delivery on the urinary bladder in the postdelivery period. Int J Gynaecol Obstet. 2010;110(2):114–7.
Musselwhite KL, Peter F, Katherine M, et al. Use of epidural anesthesia and the risk of acute postpartum urinary retention. Am J Obstet Gynecol. 2007;196(5):472 e1-72.e5.
Liang CC, Chang SD, Tseng LH, et al. Postpartum urinary retention: assessment of contributing factors and long-term clinical impact. Aust N Z J Obstet Gynaecol. 2002;42(4):365–8.
Lewis JM, Yalla SV, Stanitski KE, et al. Spectrum of urodynamic abnormalities and renal function changes in adult men with non-neurogenic urinary retention. Neurourol Urodyn. 2012;31(4):544–8.
Mustonen S, Ala-Houhala IO, Tammela TL. Long-term renal dysfunction in patients with acute urinary retention. Scand J Urol Nephrol. 2001;35(1):44–8.
Care NCCFP. Postnatal Care: Routine Postnatal Care of Women and Their Babies [Internet]. 2006.
Wilson BL, Passante T, Rauschenbach D, et al. Bladder management with epidural anesthesia during labor: a randomized controlled trial. MCN Am J Matern Child Nurs. 2015;40(4):234–42; quiz E17-8. https://doi.org/10.1097/NMC.0000000000000156.
Evron S, Dimitrochenko V, Khazin V, et al. The effect of intermittent versus continuous bladder catheterization on labor duration and postpartum urinary retention and infection: a randomized trial. J Clin Anesth. 2008;20(8):567–72. https://doi.org/10.1016/j.jclinane.2008.06.009.
Suleiman A, Mruwat-Rabah S, Garmi G, et al. Effect of intermittent versus continuous bladder catheterization on duration of the second stage of labor among nulliparous women with an epidural: a randomized controlled trial. Int Urogynecol J 2017;1–6 https://doi.org/10.1007/s00192-017-3357-9.
Alessandro L, Altman DG, Jennifer T, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Epidemiol Biostat Public Health. 2009;6(4):e1–e34.
Tian J, Zhang J, Ge L, et al. The methodological and reporting quality of systematic reviews from China and the USA are similar. J Clin Epidemiol 2017;85.
Liang Y, Rao S, Chen YL, et al. The quality of evidence in Chinese meta-analyses needs to be improved. J Clin Epidemiol. 2016;74:73–9.
Lun L, Jinhui T, Hongliang T, et al. Network meta-analyses could be improved by searching more sources and by involving a librarian. J Clin Epidemiol. 2014;67(9):1001–7.
Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ Br Med J. 2011;343(7829):889–93.
Guyatt GH, Oxman AD, Schünemann HJ, et al. GRADE guidelines: a new series of articles in the journal of clinical epidemiology. J Clin Epidemiol. 2011;64(4):380–2.
Green S. Cochrane handbook for systematic reviews of interventions: cochrane book series. Naunyn-Schmiedeberg's Arch Exp Pathol Pharmakol. 2011;5(2):S38.
Norris SL, Meerpohl JJ, Akl EA, et al. The skills and experience of GRADE methodologists can be assessed with a simple tool. J Clin Epidemiol. 2016;79:150–8.
Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan) [Computer program]. Version 5.3; 2014.
Vandenbroucke JP. Bias in meta-analysis detected by a simple, graphical test. Experts' views are still needed. BMJ Br Med J. 1997;316(7129):469–71.
Rivard C, Awad M, Liebermann M, et al. Bladder drainage during labor: a randomized controlled trial. J Obstet Gynaecol Res. 2012;38(8):1046–51. https://doi.org/10.1111/j.1447-0756.2011.01837.x.
Kerr-Wilson RHJ, McNally S. Bladder drainage for caesarean section under epidural analgesia. Br J Obstet Gynaecol. 1986;93(1):28–30.
Millet L, Shaha S, Bartholomew ML. Rates of bacteriuria in laboring women with epidural analgesia: continuous vs intermittent bladder catheterization. Am J Obstet Gynecol. 2012;206(4):316.e1-7. https://doi.org/10.1016/j.ajog.2012.02.018.
Maki DG, Tambyah PA. Engineering out the risk for infection with urinary catheters. Emerg Infect Dis. 2001;7(2):342–7.
Stamm WE. Catheter-associated urinary tract infections: epidemiology, pathogenesis, and prevention. Am J Med. 1991;91(3):65S.
Schröder UC, Bokeloh F, O'Sullivan M, et al. Guidelines on urological infections. Biomicrofluidics. 2015.
Kidd EA, Stewart F, Kassis NC, et al. Urethral (indwelling or intermittent) or suprapubic routes for short-term catheterisation in hospitalised adults. Cochrane Database Syst Rev. 2015;12(12):CD004203.
Acknowledgements
The authors thank Jinhui Tian and all members of the Evidence-Based Medicine Center, Lanzhou University, for their help with this study.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Meixuan Li, Xin Xing and Liang Yao are co-first authors
Appendices
Appendix 1 Search strategy
PubMed
#1 urinary catheters[Mesh].
#2 intermittent urethral catheter*[Mesh].
#3 urinary catheters[Title/Abstract].
#4 continuous catheter*[Title/Abstract].
#5 transurethral catheter*[Title/Abstract].
#6 transurethral tube[Title/Abstract].
#7 urinary catheter*[Title/Abstract].
#8 urinary tube[Title/Abstract].
#9 urethral catheter*[Title/Abstract].
#10 urethral tube[Title/Abstract].
#11 intermittent urethral catheter*[Title/Abstract].
#12 techniques catheter*[Title/Abstract].
#13 intermittent self catheter*[Title/Abstract].
#14 clean intermittent catheter*[Title/Abstract].
#15 clean intermittent self-catheter*[Title/Abstract].
#16 “in–out” catheter*[Title/Abstract].
#17 intermittent urethral catheter*[Title/Abstract].
#18 urethral self catheter*[Title/Abstract].
#19 clean intermittent catheter*[Title/Abstract].
#20 bladder drainage[Title/Abstract].
#21 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20.
#22 “labor, obstetric”[Mesh].
#23 labor[Title/Abstract].
#24 labour[Title/Abstract].
#25 childbirth[Title/Abstract].
#26 obstetric labor[Title/Abstract].
#27 #22 OR #23 OR #24 OR #25 OR #26 OR #27.
#28 #21 AND #27
EMBASE
#1 ‘urinary catheters’/exp.
#2 ‘intermittent urethral catheter*’[Mesh].
#3 ‘urinary catheters’: ti,ab,kw.
#4 ‘continuous catheter*’: ti,ab,kw.
#5 ‘transurethral catheter*’: ti,ab,kw.
#6 ‘transurethral tube’: ti,ab,kw.
#7 ‘urinary catheter*’: ti,ab,kw.
#8 ‘urinary tube’: ti,ab,kw.
#9 ‘urethral catheter*’: ti,ab,kw.
#10 ‘urethral tube’: ti,ab,kw.
#11 ‘intermittent urethral catheter*’: ti,ab,kw.
#12 ‘techniques catheter*’: ti,ab,kw.
#13 ‘intermittent self catheter*’: ti,ab,kw.
#14 ‘clean intermittent catheter*’: ti,ab,kw.
#15 ‘clean intermittent self-catheter*’: ti,ab,kw.
#16 ‘in–out catheter*’: ti,ab,kw.
#17 ‘intermittent urethral catheter*’: ti,ab,kw.
#18 ‘urethral self catheter*’: ti,ab,kw.
#19 ‘clean intermittent catheter*’: ti,ab,kw.
#20 ‘bladder drainage’: ti,ab,kw.
#21 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20.
#22 ‘labor, obstetric’/exp.
#23 ‘labor’: ti,ab,kw.
#24 ‘labour’: ti,ab,kw.
#25 ‘childbirth’: ti,ab,kw.
#26 ‘obstetric labor’: ti,ab,kw.
#27 #22 OR #23 OR #24 OR #25 OR #26 OR #27.
#28 #21 AND #27
Cochrane library
#1 “urinary catheters”[Mesh]).
#2 “intermittent urethral catheter*”[Mesh].
#3 urinary catheters: ti,ab,kw.
#4 continuous catheter*: ti,ab,kw.
#5 transurethral catheter*: ti,ab,kw.
#6 transurethral tube: ti,ab,kw.
#7 urinary catheter*: ti,ab,kw.
#8 urinary tube: ti,ab,kw.
#9 urethral catheter*: ti,ab,kw.
#10 urethral tube: ti,ab,kw.
#11 intermittent urethral catheter*: ti,ab,kw.
#12 techniques catheter*: ti,ab,kw.
#13 intermittent self catheter*: ti,ab,kw.
#14 clean intermittent catheter*: ti,ab,kw.
#15 clean intermittent self-catheter*: ti,ab,kw.
#16 “in–out” catheter*: ti,ab,kw.
#17 intermittent urethral catheter*: ti,ab,kw.
#18 urethral self catheter*: ti,ab,kw.
#19 clean intermittent catheter*: ti,ab,kw.
#20 bladder drainage: ti,ab,kw.
#21 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20.
#22 “labor, obstetric”[Mesh].
#23 labor: ti,ab,kw.
#24 labour: ti,ab,kw.
#25 childbirth: ti,ab,kw.
#26 obstetric labor: ti,ab,kw.
#27 #22 OR #23 OR #24 OR #25 OR #26 OR #27.
#28 #21 AND #27
Appendix 2
Rights and permissions
About this article
Cite this article
Li, M., Xing, X., Yao, L. et al. The effect of bladder catheterization on the incidence of urinary tract infection in laboring women with epidural analgesia: a meta-analysis of randomized controlled trials. Int Urogynecol J 30, 1419–1427 (2019). https://doi.org/10.1007/s00192-019-03904-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-03904-1