Abstract
Introduction and hypothesis
Urinary incontinence (UI) is frequent among women worldwide, but embarrassment and shame can prevent them from discussing symptoms with others. This study aimed to identify personal and professional relations involved by Danish women with UI. It further aimed to investigate whether age, persistence of symptoms, number of symptoms, influence on daily activities and concern about the symptoms are associated with involving personal and professional relations.
Methods
A sample of 51,090 Danish women, aged ≥ 20 years, were invited to participate in a web-based cross-sectional survey in 2012. We identified individuals with self-reported symptoms of stress incontinence, urge incontinence and UI without stress/urge and explored the involvement of personal and professional relations. Descriptive statistics and multivariate logistic regression were used for analyses.
Results
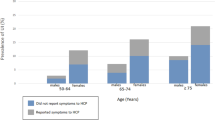
In total, 26,466 women completed the questionnaire. Of the 5861 (22.1%) women who had experienced a minimum of one UI symptom within the preceding 4 weeks, 71.4% did not involve any professional relations and 45.0% did not involve any personal relations. Further, 38.8% involved neither personal nor professional relations. Personal relations were most often involved, mainly those with the spouse/partner, friends and children. Involving a personal relation was associated with three to five times increased odds of involving health care professionals for all UI types.
Conclusions
UI is highly prevalent, but the condition is infrequently discussed in personal and professional relations. Future research should address the quality of the contacts made and barriers to involving other people.

Similar content being viewed by others
Abbreviations
- GP:
-
General practitioner
- UI:
-
Urinary incontinence
- SUI:
-
Stress urinary incontinence
- UUI:
-
Urge urinary incontinence
- HCP:
-
Health care professional
References
Minassian VA, Drutz HP, Al-Badr A. Urinary incontinence as a worldwide problem. Int J Gynaecol Obstet. 2003;82(3):327–38.
Bartoli S, Aguzzi G, Tarricone R. Impact on quality of life of urinary incontinence and overactive bladder: a systematic literature review. Urology. 2010;75(3):491–500. https://doi.org/10.1016/j.urology.2009.07.1325.
Wood LN, Anger JT. Urinary incontinence in women. BMJ. 2014;349:g4531. https://doi.org/10.1136/bmj.g4531.
Seim A, Sivertsen B, Eriksen BC, Hunskaar S. Treatment of urinary incontinence in women in general practice: observational study. BMJ. 1996;312(7044):1459–62.
The Danish College of General Practitioners (DSAM). Klinisk vejledning for almen praksis: Udredning og behandling af nedre urinvejssymptomer hos mænd og kvinder [Clinical guideline: Investigation and Treatment of Lower Urinary symptoms among Men and Women]. 2009.
Elnegaard S, Andersen RS, Pedersen AF, Larsen PV, Sondergaard J, Rasmussen S, et al. Self-reported symptoms and healthcare seeking in the general population—exploring “the symptom iceberg”. BMC Public Health. 2015;15:685. https://doi.org/10.1186/s12889-015-2034-5.
Kinchen KS, Burgio K, Diokno AC, Fultz NH, Bump R, Obenchain R. Factors associated with women's decisions to seek treatment for urinary incontinence. J Women’s Health. 2003;12(7):687–98. https://doi.org/10.1089/154099903322404339.
Elnegaard S, Pedersen AF, Sand Andersen R, Christensen Rd-P, Jarbøl DE. What triggers healthcare-seeking behaviour when experiencing a symptom? Results from a population-based survey. BJGP Open. 2017;1(2). https://doi.org/10.3399/bjgpopen17X100761.
Burgio KL, Ives DG, Locher JL, Arena VC, Kuller LH. Treatment seeking for urinary incontinence in older adults. J Am Geriatr Soc. 1994;42(2):208–12.
Roe B, Doll H, Wilson K. Help seeking behaviour and health and social services utilisation by people suffering from urinary incontinence. Int J Nurs Stud. 1999;36(3):245–53.
Shaw C, Das Gupta R, Williams KS, Assassa RP, McGrother C. A survey of help-seeking and treatment provision in women with stress urinary incontinence. BJU Int. 2006;97(4):752–7. https://doi.org/10.1111/j.1464-410X.2006.06071.x.
Holst K, Wilson PD. The prevalence of female urinary incontinence and reasons for not seeking treatment. N Z Med J. 1988;101(857):756–8.
Hagglund D, Walker-Engstrom ML, Larsson G, Leppert J. Quality of life and seeking help in women with urinary incontinence. Acta Obstet Gynecol Scand. 2001;80(11):1051–5.
Seim A, Sandvik H, Hermstad R, Hunskaar S. Female urinary incontinence—consultation behaviour and patient experiences: an epidemiological survey in a Norwegian community. Fam Pract. 1995;12(1):18–21.
Rekers H, Drogendijk AC, Valkenburg H, Riphagen F. Urinary incontinence in women from 35 to 79 years of age: prevalence and consequences. Eur J Obstet Gynecol Reprod Biol. 1992;43(3):229–34.
Pescosolido BA. Beyond rational choice: the social dynamics of how people seek help. Am J Sociol. 1992;97(4):1096–138.
Rasmussen S, Sondergaard J, Larsen PV, Balasubramaniam K, Elnegaard S, Svendsen RP, et al. The Danish symptom cohort: questionnaire and feasibility in the Nationwide study on symptom experience and healthcare-seeking among 100 000 individuals. Int J Family Med. 2014;2014:187280. https://doi.org/10.1155/2014/187280.
Pedersen CB, Gotzsche H, Moller JO, Mortensen PB. The Danish civil registration system. A cohort of eight million persons. Dan Med Bull. 2006;53(4):441–9.
Elnegaard S, Andersen RS, Pedersen AF, Jarbol DE. Activation of professional and personal network relations when experiencing a symptom: a population-based cross-sectional study. BMJ Open. 2017;7(10):e017620. https://doi.org/10.1136/bmjopen-2017-017620.
Due P, Holstein B, Lund R, Modvig J, Avlund K. Social relations: network, support and relational strain. Soc Sci Med. 1999;48(5):661–73.
Rohr G, Stovring H, Christensen K, Gaist D, Nybo H, Kragstrup J. Characteristics of middle-aged and elderly women with urinary incontinence. Scand J Prim Health Care. 2005;23(4):203–8. https://doi.org/10.1080/02813430500362803.
Schreiber Pedersen L, Lose G, Hoybye MT, Elsner S, Waldmann A, Rudnicki M. Prevalence of urinary incontinence among women and analysis of potential risk factors in Germany and Denmark. Acta Obstet Gynecol Scand. 2017. https://doi.org/10.1111/aogs.13149.
Pedersen KM, Andersen JS, Sondergaard J. General practice and primary health care in Denmark. J Am Board Fam Med. 2012;25(Suppl 1):S34–8. https://doi.org/10.3122/jabfm.2012.02.110216.
Burgio KL, Matthews KA, Engel BT. Prevalence, incidence and correlates of urinary incontinence in healthy, middle-aged women. J Urol. 1991;146(5):1255–9.
Elliott AM, McAteer A, Hannaford PC. Revisiting the symptom iceberg in today's primary care: results from a UK population survey. BMC Fam Pract. 2011;12:16. https://doi.org/10.1186/1471-2296-12-16.
Shaw C, Tansey R, Jackson C, Hyde C, Allan R. Barriers to help seeking in people with urinary symptoms. Fam Pract. 2001;18(1):48–52.
Shaw C. A review of the psychosocial predictors of help-seeking behaviour and impact on quality of life in people with urinary incontinence. J Clin Nurs. 2001;10(1):15–24.
Wojtowicz U, Plaszewska-Zywko L, Stangel-Wojcikiewicz K, Basta A. Barriers in entering treatment among women with urinary incontinence. Ginekol Pol. 2014;85(5):342–7.
Campbell SM, Roland MO. Why do people consult the doctor? Fam Pract. 1996;13(1):75–83.
Mazloomdoost D, Kanter G, Chan RC, Deveaneau N, Wyman AM, Von Bargen EC, et al. Social networking and internet use among pelvic floor patients: a multicenter survey. Am J Obstet Gynecol. 2016;215(5):654.e651–10. https://doi.org/10.1016/j.ajog.2016.06.011.
Acknowledgements
The initial survey was conducted in collaboration among the Research Unit for General Practice, University of Southern Denmark and the Research Centre for Cancer Diagnosis in Primary Care, Aarhus University.
The authors thank Sonja Wehberg and René dePont Christensen for statistical advice and calculations.
Funding
The study is financially supported by the Novo Nordisk Foundation and the Danish Cancer Society. The funding sources had no involvement in the study or in the approval of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Raasthøj, I., Elnegaard, S., Rosendal, M. et al. Urinary incontinence among women—which personal and professional relations are involved? A population-based study. Int Urogynecol J 30, 1565–1574 (2019). https://doi.org/10.1007/s00192-018-3804-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-018-3804-2