Abstract
Introduction and hypothesis
To identify the association between the symptom severity and outcome of conservative management for OAB, SUI and MUI. Conservative treatments are recommended for overactive bladder (OAB), stress urinary incontinence (SUI) and mixed incontinence (MUI). It is unclear whether disease severity affects treatment outcome.
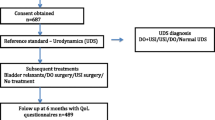
Methods
Patients receiving conservative management were reviewed. Disease-specific questionnaires (OAB-q SF, ICIQ-UI SF) and bladder diaries recorded baseline symptoms. Success was defined by Patient Global Impression of Improvement questionnaire (PGI-I) response of “very much better” or “much better”. Non-parametric statistical tests and logistic regression were used.
Results
In 50 OAB patients success was associated with lower symptom severity [30 (0–80) vs. 80 (23–100), p = 0.0001], fewer urgency episodes [4 (0–12) vs. 6 (0–11), p = 0.032] and lower ICIQ-UI SF [5.5 (0–20) vs. 15 (0–21), p = 0.002], but higher QoL [67 (20–101) vs. 24 (6–58), p = 0.0001]. In 50 MUI patients, variables were fewer urgency episodes [3 (0–10) vs. 6 (0–16), p = 0.004] and lower ICIQ-UI [11 (1–18) vs. 15 (5–21), p = 0.03]. In 40 SUI patients, variables were fewer incontinence episodes [1 (0–4) vs. 2 (0–5), p = 0.05] and lower ICIQ-UI [11 (6–16) vs. 13.5 (11–19), p = 0.003]. Multiple regression confirmed OAB-q QoL [odds ratio (OR) 1.10 (95% confidence intervals 1.04, 1.1)] for OAB, urgency episodes [OR 0.74 (0.56, 0.98)] and ICIQ-UI [OR 0.83 (0.71, 0.98] for MUI and ICIQ-UI [OR 0.57 (0.40, 0.83)] for SUI.
Conclusions
Milder baseline disease severity was associated with successful outcome. There is potential for triage at initial assessment to second-line interventions for women unlikely to achieve success.
Similar content being viewed by others
References
Irwin DE, Kopp ZS, Agatep B, Milsom I, Abrams P. Worldwide prevalence estimates of lower urinary tract symptoms, overactive bladder, urinary incontinence and bladder outlet obstruction. BJU Int. 2011;108(7):1132–8.
Milsom I, Coyne KS, Nicholson S, Kvasz M, Chen CI, Wein AJ. Global prevalence and economic burden of urgency urinary incontinence: a systematic review. Eur Urol. 2014;65(1):79–95.
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology. 2003;61:37–49.
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29:4–20.
Practice Bulletin no. 155: Urinary incontinence in women. Obstetrics and Gynecology. 2015;126(5):e66–e81.
Goldman HB, Wyndaele JJ, Kaplan SA, Wang JT. Defining response and non-response to treatment in patients with overactive bladder: a systematic review. Curr Med Res Opin. 2014;30(3):509–26.
Chapple CR, Kelleher CJ, Evans CJ, Kopp Z, Siddiqui E, Johnson N, et al. A narrative review of patient reported outcomes in overactive bladder: what is the way of the future? Eur Urol. 2016;70:799–805.
Burgio KL, Goode PS, Locher JL, Richter HE, Roth DL, Wright KC, et al. Predictors of outcome in the behavioural treatment of urinary incontinence in women. Obstet Gynecol. 2003;102:940–7.
Cammu H, van Nylen M. Pelvic floor exercises: 5 years later. Urology. 1995;45:113–8.
Burgio KL, Whitehead WE, Engel BT. Urinary incontinence in elderly: bladder sphincter biofeedback and toileting skills training. Ann Intern Med. 1985;104:507–15.
Owen RK, Abrams KR, Mayne C, Slack M, Tincello DG. Patient factors associated with Onabotulinum toxin A treatment outcome in women with detrusor overactivity. Neurourol Urodyn. 2017;36:426–31.
Schaffer J, Nager CW, Xiang F, Borello-France D, Bradley CS, Wu JM, et al. Predictors of success and satisfaction of non-surgical therapy for stress urinary incontinence. Obstet Gynecol. 2013;120(1):91–7.
Ostaszkiewicz J, Chestney T, Roe B. Habit retraining for the management of urinary incontinence in adults. Cochrane Database Syst Rev. 2004;(2):CD002801.
Wallace SA, Roe B, Williams K, Palmer M. Bladder training for urinary incontinence in adults. Cochrane Database Syst Rev. 2004;(1):CD001308.
Dumoulin C, Hay-Smith EJC, Mac Habée-Séguin G. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2014;(5):CD005654.
Jackson S, Donovan S, Brookes S, Eckford S, Swithinbank L, Abrams P. The Bristol lower urinary tract symptoms questionnaire: development and psychometric testing. BJU. 1996;77:805–12.
Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn. 2004;23(4):322–30.
Laycock J. Clinical evaluation of the pelvic floor. In: Schussler B, Laycock J, Norton P, Stanton SL, editors. Pelvic floor re-education. London: Springer-Verlag; 1994. p. 42–8.
Srikrishna S, Robinson D, Cardozo L. Validation of the patient global impression of improvement (PGI-I) for urogenital prolapse. Int Urogynecol J. 2010;21(5):523–8.
Hendriks EJ, Kessels AG, de Vet HC, Bernards AT, de Bie RA. Prognostic indicators of poor short-term outcome of physiotherapy intervention in women with stress urinary incontinence. Neurourol Urodyn. 2010;29:336–43.
Ghei M, Malone-Lee J. Using the circumstances of symptom experience to assess the severity of urgency in the OAB. J Urol. 2005;171:972–6.
Chapple C, Khullar V, Nitti VW, Frankel J, Herschorn S, Kaper M, et al. Efficacy of the beta3-adrenoreceptor agonist mirabegron for the treatment of overactive bladder by severity of incontinence at baseline: a post-hoc analysis of pooled data from three randomised phase 3 trials. Eur Urol. 2015;67:11–4.
Hsiao SM, Lin HH, Kuo HC. Factors associated with a better therapeutic effect of solifenacin in patients with overactive bladder syndrome. Neurourol Urodyn. 2014;33(3):331–4.
Serati M, Braga A, Siesto G, et al. Risk factors for the failure of antimuscarinic treatment with solifenacin in women with overactive bladder. Urology. 2013;82:1044–8.
Labrie J, Lagro-Jassen ALM, Fischer K, et al. Predicting who will undergo surgery after physiotherapy for female stress urinary incontinence. Int Urogynecol J. 2015;26:329–34.
Hendricks EJM, Kessels AGH, de Vet HCW, et al. Prognostic indicators of poor short-term outcome of physiotherapy intervention in women with stress urinary incontinence. Neurourol Urodyn. 2008;27(5):379–87.
Schaffer J, Nager CW, Xiang F, et al. Predictors of success and satisfaction of non-surgical therapy for stress urinary incontinence. Obstet Gynecol. 2012;120(1):91–7.
Klovning A, Avery K, Sandvik H, Hunskaar S. Comparison of two questionnaires for assessing the severity of urinary incontinence: the ICIQ-UI SF versus the incontinence severity index. Neurourol Urodyn. 2009;28(5):411–5.
Bo K, Larsen S. Pelvic floor muscle exercise for the treatment of female stress urinary incontinence: classification and characterisation of responders. Neurourol Urodyn. 1992;11:497–507.
Neumann PB, Grimmer KA, Deenadayalan Y. Pelvic floor muscle training and adjunctive therapies for the treatment of stress urinary incontinence in women: a systematic review. BMC Womens Health. 2006;6:11.
Knight S, Laycock J, Naylor D. Evaluation of neuromuscular electrical stimulation in the treatment of genuine stress incontinence. Physiotherapy. 1998;84(2):61–71.
Turkan A, Inci Y, Fazli D. The short-term effects of physical therapy in different intensities of urodynamic stress incontinence. Gynecol Obstet Investig. 2005;59:43–8.
Dumoulin C, Desmeule F, Hagen S, Masse BR, Mayrand M-H, Morin M, et al. Development and validation of a clinical prediction rule to guide and improve the treatment of female stress urinary incontinence. http://webapps.cihr-irsc.gc.ca/decisions/p/project_details.html?applId=344799&lang=en. Accessed 13 Apr 2018.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This work took place at the Leicester General Hospital NHS Trust, UK.
No ethical approval was required for this work.
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Obloza, A., Teo, R., Marriott, E. et al. Association of baseline severity of lower urinary tract symptoms with the success conservative therapy for urinary incontinence in women. Int Urogynecol J 30, 705–710 (2019). https://doi.org/10.1007/s00192-018-3778-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-018-3778-0