Abstract
Introduction and hypothesis
A rectocele is the bulging of the anterior rectal wall into the posterior vaginal compartment. The route of surgical repair can be transvaginal, transrectal or abdominal. The aim of this retrospective study is to describe a novel transvaginal surgical procedure and investigate the associated subjective and objective clinical outcomes.
Methods
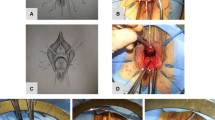
Database records were retrieved for all women who underwent a rectocele plication for the period from January 2010 until December 2015 in a referral urogynecology unit with a minimum follow-up period of 12 months. This transvaginal technique entails a plication of the anterior rectal wall by suturing of the rectal muscularis layer. Clinical findings and quality of life (QOL) metrics were evaluated and reported on.
Results
One hundred thirty-nine women met the initial inclusion criteria with full data available for 123. The presenting symptoms included a vaginal bulge in 73 (52.5%), overactive bladder (OAB) in 73 (52.5%), obstructed defecation (OD) in 49 (35.3%) and anal incontinence (AI) in 35 (25.2%). The majority of women (n = 72, 51.8%) had stage 3–4 posterior prolapse. The mean follow-up period was 27 ± 15 months. The postoperative symptoms were significantly improved for all, except AI (p = 0.43). There was a significant improvement in posterior prolapse (p < 0.001) with the majority of women noted to have a stage 0 or 1 (n = 109; 88.6%) posterior prolapse at follow-up.
Conclusions
The rectocele plication is a novel surgical technique with good subjective and objective clinical outcomes in the medium term.

Similar content being viewed by others
References
Wu JM, Matthews CA, Conover MM, Pate V, Jonsson FM. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014;123(6):1201–6.
Karram M, Maher C. Surgery for posterior vaginal wall prolapse. Int Urogynecol J. 2013;24(11):1835–41.
Maher C, Baessler K. Surgical management of posterior vaginal wall prolapse: an evidence-based literature review. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17(1):84–8.
Leanza V, Intagliata E, Leanza G, Cannizzaro MA, Zanghì G, Vecchio R. Surgical repair of rectocele. Comparison of transvaginal and transanal approach and personal technique. G Chir. 2013;34(11–12):332–6.
Kleeman SD, Karram M. Posterior pelvic floor prolapse and a review of the anatomy, preoperative testing and surgical management. Minerva Ginecol. 2008;60(2):165–82.
Boccasanta P, Venturi M, Calabrò G, Trompetto M, Ganio E, Tessera G, et al. Which surgical approach for rectocele? A multicentric report from Italian coloproctologists. Tech Coloproctol. 2001;5(3):149–56.
Maher C, Feiner B, Baessler K, Schmid C. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013;4:CD004014.
Glavind K, Christiansen AG. Site-specific colporrhaphy in posterior compartment pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2016;27(5):735–9.
Richardson AC. The rectovaginal septum revisited: its relationship to rectocele and its importance in rectocele repair. Clin Obstet Gynecol. 1993;36(4):976–83.
Regadas FSP, Lima Barreto RG, Murad-Regadas SM, Veras Rodrigues L, Pereira Oliveira LM. Correlation between anorectocele with the anterior anal canal and anorectal junction anatomy using echodefecography. Tech Coloproctol. 2012;16(2):133–8.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335(7624):806–8.
Haylen BT, Maher CF, Barber MD, Camargo S, Dandolu V, Digesu A, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic organ prolapse (POP). Int Urogynecol J. 2016;27(4):655–84.
Dietz HP. Ultrasound imaging of the pelvic floor. Part I: two-dimensional aspects. Ultrasound Obstet Gynecol. 2004;23(1):80–92.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96.
Henn EW, Nondabula T, Juul L. Effect of vaginal infiltration with ornipressin or saline on intraoperative blood loss during vaginal prolapse surgery: a randomised controlled trial. Int Urogynecol J. 2016;27(3):407–12.
Abramov Y, Gandhi S, Goldberg RP, Botros SM, Kwon C, Sand PK. Site-specific rectocele repair compared with standard posterior colporrhaphy. Obstet Gynecol. 2005;105(2):314–8.
Goh JTW, Tjandra JJ, Carey MP. How could management of rectoceles be optimized? ANZ J Surg. 2002;72(12):896–901.
Brown H, Grimes C. Current trends in management of defecatory dysfunction, posterior compartment prolapse, and fecal incontinence. Curr Obstet Gynecol Rep. 2016;5(2):165–71.
Dietz HP, Korda A. Which bowel symptoms are most strongly associated with a true rectocele? Aust N Z J Obstet Gynaecol. 2005;45(6):505–8.
Hall G, Shanmugan S, Nobel T, Paspulati R, Delaney C, Reynolds H, et al. Symptomatic rectocele: what are the indications for repair? Am J Surg. 2014;207(3):375–9.
Riss S, Stift A. Surgery for obstructed defecation syndrome—is there an ideal technique. World J Gastroenterol. 2015;21(1):1–5.
Hicks CW, Weinstein M, Wakamatsu M, Savitt L, Pulliam SBL. In patients with rectoceles and obstructed defecation syndrome, surgery should be the option of last resort. Surgery. 2014;155(4):659–67.
Pescatori M, Spyrou M, Pulvirenti d’Urso A. A prospective evaluation of occult disorders in obstructed defecation using the “iceberg diagram”. Color Dis. 2006;8(9):785–9.
Basu M, Wise B, Duckett J. Urgency resolution following prolapse surgery: is voiding important? Int Urogynecol J. 2013;24(8):1309–13.
Miranne JM, Lopes V, Carberry CL, Sung VW. The effect of pelvic organ prolapse severity on improvement in overactive bladder symptoms after pelvic reconstructive surgery. Int Urogynecol J. 2013;24(8):1303–8.
Beck DE, Allen NL. Rectocele. Clin Colon Rectal Surg. 2010;23(2):90–8.
Luo J, Chen L, Fenner DE, Ashton-Miller JA, Delancey JOL. A multi-compartment 3-D finite element model of rectocele and its interaction with cystocele. J Biomech. 2015;48(9):1580–6.
Albuquerque A, Pereira E. Current applications of transperineal ultrasound in gastroenterology. World J Radiol. 2016;8(4):370–8.
Tsunoda A, Ohta T, Kiyasu Y, Kusanagi H. Laparoscopic ventral Rectopexy for Rectoanal intussusception. Dis Colon Rectum. 2015;58(4):449–56.
Thompson JR, Chen AH, Pettit PDM, Bridges MD, Paraiso MFR. Incidence of occult rectal prolapse in patients with clinical rectoceles and defecatory dysfunction. Am J Obstet Gynecol. 2002;187(6):1494–500.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Conference presentation
RCOG World Congress, Cape Town, 20–22 March 2017
IUGA annual meeting, Vancouver, 20–24 June 2017
Rights and permissions
About this article
Cite this article
Henn, E.W., Cronje, H.S. Rectocele plication: description of a novel surgical technique and review of clinical results. Int Urogynecol J 29, 1655–1660 (2018). https://doi.org/10.1007/s00192-018-3623-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-018-3623-5