Abstract
Introduction and hypothesis
The use of mesh for vaginal prolapse gained popularity during the 1990s. More recently, concerns have been raised regarding the safety of mesh procedures. Mesh can be inserted vaginally, laparoscopically or via an open abdominal route, but there are few data comparing the outcomes. Most previous published data relate to small numbers of procedures.
Methods
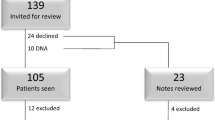
This was a review of data submitted to the British Society of Urogynaecology (BSUG) database of all cases reporting the use of mesh placed vaginally or abdominally (open or laparoscopic) between January 2006 and December 2016. The primary outcome was based on the reported patient global impression of improvement (PGI-I).
Results
A total of 6,709 cases of mesh prolapse repair were entered during the study period. Women in the laparoscopic group had a lower BMI and were younger. Significantly more patients in the open group (96.4%) described themselves as very much better or much better compared with the laparoscopic group (91%) and the vaginal mesh group (90.7%; p < 0.001). Only 0.5% of patients reported that they were worse or very much worse.
Conclusions
This dataset suggests that the effectiveness of mesh repair might be good regardless of the route of insertion. The improvement in PGI-I seems to be greatest with open sacrocolpopexy.

Similar content being viewed by others
References
Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Brown J. Surgery for women with anterior compartment prolapse. Cochrane Database Syst Rev. 2016; https://doi.org/10.1002/14651858.CD004014.pub6.
FDA Public Health Notification: serious complications associated with transvaginal placement of surgical mesh in repair of pelvic organ prolapse and stress urinary incontinence. 2008. http://www.fda.gov/cdrh/consumer/surgicalmesh-popsui.html.
The Scottish Independent Review of the use, safety and efficacy of transvaginal mesh implants in the treatment of stress urinary incontinence and pelvic organ prolapse in women: Interim Report. 2015. www.gov.scot/publications/2015/10/8485.
Dandolu V, Akiyama M, Allenback G, Pathak P. Mesh complications and failure rates after transvaginal mesh repair compared with abdominal or laparoscopic sacrocolpopexy and to native tissue repair in treating apical prolapse. Int Urogynecol J. 2017;28(2):215–22.
Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Brown J. Surgery for women with apical vaginal prolapse. Cochrane Database Syst Rev. 2016; https://doi.org/10.1002/14651858.CD012376.
Sacrocolpopexy using mesh for vaginal vault prolapse repair. Interventional Procedures Guidance [IPG283]. 2009. https://www.nice.org.uk/guidance/ipg283/chapter/1-guidance.
Constantini E, Mearini L, Lazzeri M, Bini V, Nunzi E, di Biase MM, et al. Laparoscopic vs abdominal sacrocolpopexy: a randomized controlled trial. J Urol. 2016;196(1):159–65.
Freeman RM, Pantazis K, Thomson A, Frappell J, Bombieri L, Moran P, et al. A randomized controlled trial of abdominal versus laparoscopic sacrocolpopexy for the treatment of post-hysterectomy vaginal vault prolapse: LAS study. Int Urogynecol J. 2013;24(3):377–84.
Khan A, Alperin M, Wu N, Clemes JQ, Dubina E, Pashos CL, et al. Comparative outcomes of open versus laparoscopic sacrocolpopexy among Medicare beneficiaries. Int Urogynecol J. 2013;24(11):1883–91.
Gupta P, Payne J, Killinger KA, Ehlert M, Bartley J, Guilleran J, et al. Analysis of changes in sexual function in women undergoing pelvic organ prolapse repair with abdominal or vaginal approaches. Int Urogynecol J. 2016;27(12):1919–24.
Gutman RE, Rardin CR, Sokol ER, Matthews C, Park AJ, Iglesia CB, et al. Vaginal and laparoscopic mesh hysteropexy for uterovaginal prolapse: a parallel cohort study. Am J Obstet Gynecol. 2017;216(1):38.e1–38.e11.
Glazener CM, Breeman S, Elders A, Hemming C, Cooper KG, Freeman RM, et al. Mesh, graft or standard repair for women having primary transvaginal anterior or posterior compartment prolapse surgery: two parallel-group, multicenter, randomized, controlled trials (PROSPECT). Lancet. 2017;389(10067):381–92.
Acknowledgements
The authors would like to thank the members of the British Society of Urogynaecology who contribute their data to the database, and its Research Committee for granting access to the data.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflicts of interest
RDT has received travel expenses and/or honoraria from Boston Scientific, Pfizer, Astellas and Covidien. He is a member of the BSUG General Committee.
Steven Lane has no conflicts of interest to declare.
Jonathan Duckett has received travel expenses and/or honoraria from Astellas, Ethicon, Pfizer, Lilly, Boston and Syner Med. He is Vice Chairman of BSUG and member of the IUJ Editorial Board.
Rights and permissions
About this article
Cite this article
Trochez, R.D., Lane, S., Duckett, J. et al. The use of synthetic mesh for vaginal prolapse in the UK: a review of cases submitted to the British Society of Urogynaecology database. Int Urogynecol J 29, 899–904 (2018). https://doi.org/10.1007/s00192-018-3595-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-018-3595-5