Abstract
Introduction and hypothesis
Numerous studies have found that the short-term results of laparoscopic sacrocolpopexy for pelvic organ prolapse are safe and effective. This study evaluates the long-term results of the laparoscopic sacrocolpopexy operation between the urology and gynecology branches.
Methods
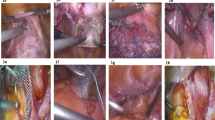
A prospective study enrolling 206 patients was conducted to evaluate laparoscopic sacrocolpopexy as a surgical treatment for vaginal vault prolapse from 2011 to 2014. Two different surgical branches (urology and gynecology) applied laparoscopic sacrocolpopexy to their patients with their own techniques. The long-term results were assessed postoperatively after 4 years by pelvic examinations, including the Pelvic Organ Prolapse Quantification system (POP-Q) and quality-of-life assessments using validated questionnaires.
Results
A total of 190 patients (94 urology and 96 gynecology patients) received a full clinical follow-up examination between April 2014–June 2018. Postoperative pelvic organ prolapse recurrence rates in each compartment were similar in both groups during the 4 years; 87.2% of the urology and 86.5% of the gynecology patients had no prolapse in any compartment according to the POP-Q system. The reoperation rate was 5.3% for the urology and 6.2% for the gynecology group. Mesh erosion was detected in two patients in both groups. Three patients responded to local estrogen therapy, and we removed the mesh vaginally in one patient. The subjective cure rate was 89.4% in the urology and 88.5% in the gynecology group after 4 years.
Conclusions
Although different surgical branches perform laparoscopic sacrocolpopexy with their own techniques, long-term anatomical and functional results are similar between the branches. From a urogynecological point of view, laparoscopic sacrocolpopexy is a gold standard surgical procedure that can be performed by both urologists and gynecologists with similar long-term outcomes.


Similar content being viewed by others
References
Wu JM, Hundley AF, Fulton RG, Myers ER. Forecasting the prevalence of pelvic floor disorders in US women: 2010 to 2050. Obstet Gynecol. 2009;114:1278.
Jones KA, Shepherd JP, Oliphant SS, Wang L, Bunker CH, Lowder JL. Trends in inpatient prolapse procedures in the United States, 1979–2006. Am J Obstet Gynecol. 2010;202(5):501.e1–7.
Cvach K, Dwyer P. Surgical management of pelvic organ prolapse: abdominal and vaginal approaches. World J Urol. 2012;30(4):471–7. https://doi.org/10.1007/s00345-011-0776-y.
Altman D, Väyrynen T, Engh ME, Axelsen S, Falconer C, et al. Anterior colporrhaphy versus transvaginal mesh for pelvic-organ prolapse. N Engl J Med. 2011;364(19):1826–36.
Nieminen K, Hiltunen R, Takala T, Heiskanen E, Merikari M, Niemi K, et al. Outcomes after anterior vaginal wall repair with mesh: a randomized, controlled trial with a three-year follow-up. Am J Obstet Gynecol. 2010;203(3):235.e1–8.
Nguyen JN, Burchette RJ. Outcome after anterior vaginal prolapse repair: a randomized controlled trial. Obstet Gynecol. 2008;111(4):891–8.
UPDATE on Serious Complications Associated with Transvaginal Placement of Surgical Mesh for Pelvic Organ Prolapse, FDA, July 2011 https://www.fda.gov/downloads/medicaldevices/safety/alertsandnotices/ucm262760.pdf. Accessed 26 Oct 2018.
Gomelsky A, Dmochowski RR. Vaginal mesh update. Curr Opin Urol. 2012;22(4):271–5.
Coolen AWM, van Oudheusden AMJ, Mol BWJ, van Eijndhoven HWF, Roovers JWR, Bongers MY. Laparoscopic sacrocolpopexy compared with open abdominal sacrocolpopexy for vault prolapse repair: a randomized controlled trial. Int Urogynecol J. 2017;28(10):1469–79.
Geller EJ, Siddiqui NY, Wu JM, Visco AG. Short-term outcomes of robotic sacrocolpopexy compared with abdominal sacrocolpopexy. Obstet Gynecol. 2008;112:1201.
Lane FE. Repair of posthysterectomy vaginal-vault prolapse. Obstet Gynecol. 1962;20:72–7.
Anand M, Weaver AL, Fruth KM, et al. Perioperative complications and cost of vaginal, open abdominal, and robotic surgery for apical vaginal vault prolapse. Female Pelvic Med Reconstr Surg. 2017;23:27.
Maher C, Feiner B, Baessler K, Schmid C. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013:CD004014.
De Gouveia De Sa M, Claydon LS, Whitlow B, Dolcet Artahona MA. Laparoscopic versus open sacrocolpopexy for treatment of prolapse of the apical segment of the vagina: a systematic review and meta-analysis. Int Urogynecol J. 2016;27(1):3–17.
Patel M, O’Sullivan D. Tulikangas PK. A comparison of costs for abdominal, laparoscopic, and robot-assisted sacral colpopexy. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:223.
Judd JP, Siddiqui NY, Barnett JC, et al. Cost-minimization analysis of robotic-assisted, laparoscopic, and abdominal sacrocolpopexy. J Minim Invasive Gynecol. 2010;17:493.
Freeman RM, Pantazis K, Thomson A, Frappell J, Bombieri L, Moran P, et al. A randomized controlled trial of abdominal versus laparoscopic sacrocolpopexy for the treatment of post-hysterectomy vaginal vault prolapse: LAS study. Int Urogynecol J. 2013;24(3):377–84.
Paraiso MF, Jelovsek JE, Frick A, et al. Laparoscopic compared with robotic sacrocolpopexy for vaginal prolapse: a randomized controlled trial. Obstet Gynecol. 2011;118:1005.
Anger JT, Mueller ER, Tarnay C, et al. Robotic compared with laparoscopic sacrocolpopexy: a randomized controlled trial. Obstet Gynecol. 2014;123:5.
Bump RC, Mattiasson A, Bø K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7.
Kaplan PB, Sut N, Sut HK. Validation, cultural adaptation and responsiveness of two pelvic-floor-specific quality-of-life questionnaires, PFDI-20 and PFIQ-7, in a Turkish population. Eur J Obstet Gynecol Reprod Biol. 2012;162(2):229–33.
Coolen AWM, Bui BN, Dietz V, Wang R, van Montfoort APA, Mol BWJ, et al. The treatment of post-hysterectomy vaginal vault prolapse: a systematic review and meta-analysis. Int Urogynecol J. 2017;28(12):1767–83.
Maher CF, Feiner B, DeCuyper EM, Nichlos CJ, Hickey KV, O’Rourke P. Laparoscopic sacral colpopexy versus total vaginal mesh for vaginal vault prolapse: a randomized trial. Am J Obstet Gynecol. 2011;204(4):360.e1–7.
Sarlos D, Kots L, Ryu G, Schaer G. Long-term follow-up of laparoscopic sacrocolpopexy. Int Urogynecol J. 2014;25(9):1207–12.
Hilger WS, Poulson M, Norton PA. Long-term results of abdominal sacrocolpopexy. Am J Obstet Gynecol. 2003;189:1606.
Nygaard I, Brubaker L, Zyczynski HM, et al. Long-term outcomes following abdominal sacrocolpopexy for pelvic organ prolapse. JAMA. 2013;309:2016.
Trabuco EC, Linder BJ, Klingele CJ, Blandon RE, Occhino JA, Weaver AL, et al. Two-year results of Burch compared with midurethral sling with sacrocolpopexy: a randomized controlled trial. Obstet Gynecol. 2018;131(1):31–8.
Nygaard IE, McCreery R, Brubaker L. Abdominal sacrocolpopexy: a comprehensive review. Obstet Gynecol. 2004;104:805.
Nair R, Nikolopoulos KI, Claydon LS. Clinical outcomes in women undergoing laparoscopic hysteropexy: a systematic review. Eur J Obstet Gynecol Reprod Biol. 2017;208:71.
Jeon MJ, Jung HJ, Choi HJ, et al. Is hysterectomy or the use of graft necessary for the reconstructive surgery for uterine prolapse? Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:351.
Acknowledgments
The authors thank our residents for their help in collecting the data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Orhan, A., Ozerkan, K., Vuruskan, H. et al. Long-term follow-up of laparoscopic sacrocolpopexy: comparison of two different techniques used in urology and gynecology. Int Urogynecol J 30, 623–632 (2019). https://doi.org/10.1007/s00192-018-03858-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-018-03858-w