Abstract
Introduction and hypothesis
The aim of this study was to assess the safety and efficacy of vaginal native tissue repair and uterine suspension after a follow-up of at least 1 year.
Methods
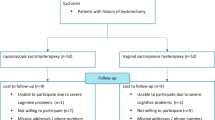
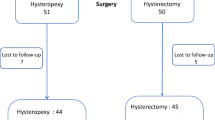
We included all consecutive women with an anterior vaginal prolapse of stage II or higher and a concomitant uterine prolapse of stage II who underwent this surgical procedure. We considered women with a descensus with maximum point of less than −1 in any compartment as objectively cured. Overall success was defined as no prolapse symptoms, together with a Patient Global Impression of Improvement (PGI-I) score of 2 or less, prolapse of stage lower than II, and no need for other surgery.
Results
A total of 102 patients underwent this surgical procedure during the study period and met all the inclusion criteria for statistical analysis. The mean follow-up was 31 ± 8.2 months; no patient was lost to follow-up. Five patients (4.9%) showed postoperative complications. In terms of subjective outcomes, at the last available follow-up, failure of this surgical procedure was seen in 2% of patients. The objective cure rate and the overall cure rate were the 95.1%. No significant deterioration in objective cure rates was observed over time (p = 0.6).
Conclusions
Vaginal repair and hysteropexy appear to be an effective and safe option for women with advanced uterovaginal prolapse.
Similar content being viewed by others
References
Slieker-ten Hove MC, Pool-Goudzwaard AL, Eijkemans MJ, Steegers-Theunissen RP, Burger CW, Vierhout ME. The prevalence of pelvic organ prolapse symptoms and signs and their relation with bladder and bowel disorders in a general female population. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:1037–45.
Luber KM, Boero S, Choe JY. The demographics of pelvic floor disorders: current observations and future projections. Am J Obstet Gynecol. 2001;184:1496–501.
Wu JM, Hundley AF, Fulton RG, et al. Forecasting the prevalence of pelvic floor disorders in U.S. women: 2010 to 2050. Obstet Gynecol. 2009;114:1278–83.
Detollenaere RJ, den Boon J, Stekelenburg J, IntHout J, Vierhout ME, Kluivers KB, et al. Sacrospinous hysteropexy versus vaginal hysterectomy with suspension of the uterosacral ligaments in women with uterine prolapse stage 2 or higher: multicentre randomised non-inferiority trial. BMJ. 2015;351:h3717.
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89:501–6.
Detollenaere RJ, den Boon J, Kluivers KB, Vierhout ME, van Eijndhoven HW. Surgical management of pelvic organ prolapse and uterine descent in the Netherlands. Int Urogynecol J. 2013;24:781–8.
Korbly NB, Kassis NC, Good MM, et al. Patient preferences for uterine preservation and hysterectomy in women with pelvic organ prolapse. Am J Obstet Gynecol. 2013;209:470.e1–6.
Maher CF, Cary MP, Slack MC, Murray CJ, Milligan M, Schluter P. Uterine preservation or hysterectomy at sacrospinous colpopexy for uterovaginal prolapse? Int Urogynecol J Pelvic Floor Dysfunct. 2001;12:381–4.
Huffaker RK, Kuehl TJ, Muir TW, Yandell PM, Pierce LM, Shull BL. Transverse cystocele repair with uterine preservation using native tissue. Int Urogynecol J. 2008;19:1275–81.
Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21:5–26.
Schafer W, Abrams P, Liao L, et al. Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn. 2002;21:261–74.
Srikrishna S, Robinson D, Cardozo L. Validation of the Patient Global Impression of Improvement (PGI-I) for urogenital prolapse. Int Urogynecol J. 2010;21:523–8.
Chmielewski L, Walters MD, Weber AM, Barber MD. Reanalysis of a randomized trial of 3 techniques of anterior colporrhaphy using clinically relevant definitions of success. Am J Obstet Gynecol. 2011;205:69.e1–8.
Digesu GA, Khullar V, Cardozo L, Robinson D, Salvatore S. P-QOL: a validated questionnaire to assess the symptoms and quality of life of women with urogenital prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16:176–81.
Digesu GA, Santamato S, Khullar V, et al. Validation of an Italian version of the prolapse quality of life questionnaire. Eur J Obstet Gynecol Reprod Biol. 2003;106:184–92.
Baden WF, Walker T. Surgical repair of vaginal defects. Philadelphia: Lippincott; 1992.
Madhu C, Foon R, Agur W, Smith P. Does traction on the cervix under anaesthesia tell us when to perform a concomitant hysterectomy? A 2-year follow-up of a prospective cohort study. Int Urogynecol J. 2014;25:1213–7.
Serati M, Rizk D, Savatore S. In the footsteps of Bonney and Nichols: hysterectomy during surgical repair of pelvic organ prolapse. Int Urogynecol J. 2017;28:823–5.
Gutman R, Maher C. Uterine-preserving POP surgery. Int Urogynecol J. 2013;24:1803–13.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Serati, M., Braga, A., Cantaluppi, S. et al. Vaginal cystocele repair and hysteropexy in women with anterior and central compartment prolapse: efficacy and safety after 30 months of follow-up. Int Urogynecol J 29, 831–836 (2018). https://doi.org/10.1007/s00192-017-3498-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-017-3498-x