Abstract
Introduction and hypothesis
To determine the prevalence of levator ani (LA) muscle subdivision defects in patients with SUI using three-dimensional endovaginal ultrasound (3D EVUS).
Methods
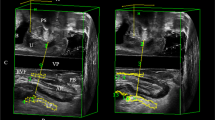
This is a prospective cohort study of 100 patients with pure or predominant urodynamic SUI who underwent 3D EVUS. The 3D cubes obtained were analyzed and the LA muscle was divided into three subgroups: the puboperinealis/puboanalis, the puborectalis, and the iliococcygeus/pubococcygeus. Each LA muscle subdivision was individually scored on each side (0: no defect, 1: ≤50 % muscle loss, 2: > 50 % muscle loss, and 3: total absence of the muscle) and a cumulative score, categorized as 0 (no defect), mild (total score 1–6), moderate (7–12), and severe (≥13) was calculated.
Results
The number of women with no LA muscle defect or a mild defect was significantly higher than the number of those with a moderate or severe defect (p < 0.001). Apart from the small inverse relationship of the total puborectalis muscle score and the cumulative subdivision score with maximal urethral closure pressure (r value > −0.3; p < 0.05), the muscle defect scores were not found to correlate with urodynamic parameters (p > 0.05). Although all muscle subdivisions contributed to the overall LA muscle defect score, the association was strongest for the puborectalis component (r = 0.9; p < 0.001). The prevalence of the LA muscle defect in patients with intrinsic sphincter deficiency (ISD) was not significantly different from that in patients without ISD.
Conclusion
Patients with SUI have a higher prevalence of no or mild LA defect compared with a moderate or severe LA defect.


Similar content being viewed by others
References
Mant J, Painter R, Vessey M (1997) Epidemiology of genital prolapse: observations from the Oxford Family Planning Association Study. Br J Obstet Gynaecol 104:579–585
Rortveit G, Hannestad YS, Daltveit AK, Hunskaar S (2001) Age- and type-dependent effects of parity on urinary incontinence: the Norwegian EPINCONT study. Obstet Gynecol 98:1004–1010
Kearney R, Miller JM, Ashton-Miller JA, DeLancey JOL (2006) Obstetrical factors associated with levator ani muscle injury after vaginal birth. Obstet Gynecol 107(1):144–149
Dietz HP, Lanzarone V (2005) Levator trauma after vaginal delivery. Obstet Gynecol 106(4):707–712
Svabik K, Shek KL, Dietz HP (2009) How much does the levator hiatus have to stretch during childbirth? BJOG 116(12):1657–1662
DeLancey J, Morgan D, Fenner D, Kearney R, Guire K, Miller JM et al (2007) Comparison of levator ani muscle defects and function in women with and without pelvic organ prolapse. Obstet Gynecol 109:295–302
Dietz HP, Steensma AB (2006) The prevalence of major abnormalities of the levator ani in urogynaecological patients. BJOG 113:225–230
Adekanmi OA, Freeman RM, Jackson SA, Puckett M, Bombieri L, Waterfield MR (2009) Do the anatomical defects associated with cystocele affect the outcome of the anterior repair? A clinical and radiological study. Int Urogynecol J Pelvic Floor Dysfunct 20(11):1369–1377
Rortveit G, Subak LL, Thom DH, Creasman JM, Vittinghoff E, Van Den Eeden SK, Brown JS (2010) Urinary incontinence, fecal incontinence and pelvic organ prolapse in a population-based, racially diverse cohort: prevalence and risk factors. Female Pelvic Med Reconstr Surg 16(5):278–283
DeLancey JOL, Kearney R, Chou Q, Speights S, Binno S (2003) The appearance of levator ani muscle abnormalities in magnetic resonance images after vaginal delivery. Obstet Gynecol 101(1):46–53
Dietz HP, Kirby A, Shek KL, Bedwell PJ (2009) Does avulsion of the puborectalis muscle affect bladder function? Int Urogynecol J 20:967–972
Morgan DM, Cardoza P, Guire K, Fenner DE, DeLancey JOL (2010) Levator ani defect status and lower urinary tract symptoms in women with pelvic organ prolapse. Int Urogynecol J 21:47–52
Shobeiri SA, LeClaire E, Nihira MA, Quiroz LH, O’Donaghue D (2009) Appearance of the levator ani muscle subdivisions in endovaginal three-dimensional ultrasonography. Obstet Gynecol 114:66–72
Shobeiri SA, Rostaminia G, White D, Hegde A, Mukati M, Quiroz L (2012) How much levator muscle defect is associated with female pelvic organ prolapse? Int Urogynecol J 23(S2):S163
Dietz HP, Simpson JM (2008) Levator trauma is associated with pelvic organ prolapse. BJOG 115:979–984
Derpapas A, Digesu AG, Hamady M, Gallo P, Dell’Utri C, Vijaya G, Khullar V (2013) Prevalence of pubovisceral muscle avulsion in a general gynecology cohort: a computed tomography study. Neurourol Urodyn 32(4):359–362
DeLancey JOL (1997) The pathophysiology of stress urinary incontinence and its implications for surgical treatment. World J Urol 15:268–274
Muellner SR (1951) Physiology of micturition. J Urol 65:805–810
Parks AG, Porter NH, Melzak (1962) Experimental study of the reflex mechanism controlling muscles of the pelvic floor. Dis Colon Rectum 5:407–414
Hanzal E, Berger E, Koelbl H (1993) Levator ani muscle morphology and recurrent genuine stress incontinence. Obstet Gynecol 81:426–429
Snooks SJ, Badenoch DF, Tiptaft RC, Swash M (1985) Perineal nerve damage in genuine stress urinary incontinence. An electrophysiological study. Br J Urol 57:422–426
Smith AR, Hosker GL, Warrell DW (1989) The role of partial denervation of the pelvic floor in the aetiology of genitourinary prolapse and stress incontinence of urine. A neurophysiological study. Br J Obstet Gynaecol 96(1):29–32
Sajadi KP, Lin DL, Steward JE, Balog B, Dissaranan C, Zaszczurynski P, Gill BC, Jiang HH, Kerns JM, Damaser MS (2012) Pudendal nerve stretch reduces external urethral sphincter activity in rats. J Urol 188(4):1389–1395
Bakas P, Liapis A, Karanreas A, Creatsas G (2001) Pudendal nerve terminal motor latency in women with genuine stress incontinence and prolapse. Gynecol Obstet Invest 51:187–190
Da Silva AS, Digesu A, Dell’Utri C, Fritsch H, Piffarotti P, Khullar V (2015) Do ultrasound findings of levator ani “avulsion” correlate with anatomical findings: a multicenter cadaveric study. Neurourol Urodyn DOI: 10.1002/nau.22781
Kapoor DS, Housami F, White P, Swithinbank L, Drake M (2012) Maximum urethral closure pressure in women: normative data and evaluation as a diagnostic test. Int Urogynecol J 23(11):1613–1618
Goepel C, Thomssen C (2006) Changes in the extracellular matrix in periurethral tissue of women with stress urinary incontinence. Acta Histochem 108(960):441–445
Javadian P, O’Leary D, Rostaminia G et al (2015) How does 3D endovaginal ultrasound compare to magnetic resonance imaging in the evaluation of levator ani anatomy? Neurourol Urodyn DOI: 10.1002/nau.22944
Lien KC, Mooney B, DeLancey JO (2004) Levator ani muscle stretch induced by simulated vaginal birth. Obstet Gynecol 103:31–40
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hegde, A., Aguilar, V.C. & Davila, G.W. Levator ani defects in patients with stress urinary incontinence: three-dimensional endovaginal ultrasound assessment. Int Urogynecol J 28, 85–93 (2017). https://doi.org/10.1007/s00192-016-3068-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-016-3068-7