Abstract
Introduction and hypothesis
Pelvic floor muscle training (PFMT) is widely recommended as first-line therapy for women with urinary incontinence. However, adherence to PFMT decreases over time, and information regarding barriers to PFMT is scarce. The primary aim of our study was to investigate whether a vaginal spheres device helped improve adherence to PFMT. The secondary aim was to assess determinants of adherence and the association with treatment outcome.
Methods
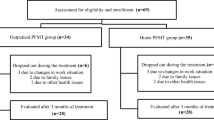
This was a secondary analysis of a randomized trial with a 6-month follow-up in women with urinary incontinence (UI) in whom we evaluated adherence to PFMT, performed either with (spheres group) or without (control group) vaginal spheres. The Morisky-Green Questionnaire (MGQ) was used to assess adherence, defined as the extent to which participants corresponded to the agreed recommendations; participants were classified as adherent or nonadherent according to their responses. Efficacy of PFMT was assessed using the International Consultation on Incontinence Questionnaire Short Form scale (ICIQ-SF).
Results
Seventy women were enrolled and data from 65 (35 treated and 30 controls) were suitable for analysis. There were no significant differences in adherence to treatment between groups at the end of follow-up (33.3 % in controls and 42.9 % in spheres). The largest group of nonadherent women in both arms were those who mainly forgot to do the exercises. ICIQ-SF results between adherent and nonadherent women did not differ significantly [mean 0.55, 95 % confidence interval (CI) 1.13–2.25]. No significant difference was observed between women who attained greater and lesser improvement in UI after treatment (4.5 %; 95 % CI −11.7 to 20.6).
Conclusions
In patients with UI, vaginal spheres as an adjunct to PFMT did not increase adherence to pelvic muscle exercises. Lack of persistence appeared to be due to forgetfulness and did not seem to be influenced by the efficacy of PFMT.



Similar content being viewed by others
References
Nygaard I, Barber MD, Burgio KL et al (2008) Prevalence of symptomatic pelvic floor disorders in US women. JAMA 300:1311–1316
Norton P, Brubaker L (2006) Urinary incontinence in women. Lancet 367:57–67
Dumoulin C, Hay-Smith J (2010) Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev 1, CD005654
Moore K, Dumoulin C, Bradley C, Burgio K, Chambers T, Hagen S, et al. Adult conservative management. In: Abrams P, Cardozo L, Khy S, Wein A, editors. Incontinence, 5th edition. ICUD-EAU 2013. Committee 12: 1101–1175
Bo K (2004) Pelvic floor muscle training is effective in treatment of female stress urinary incontinence, but how does it work? Int Urogynecol J 15:76–84. doi:10.1007/s00192-004-1125-0
Bo K, Hilde G (2013) Does it work in the long term?—a systematic review on pelvic floor muscle training for female stress urinary incontinence. Neurourol Urodyn 32:215–223
Imamura M, Abrams P, Bain C, Buckley B, Cardozo L, Cody J et al (2010) Systematic review and economic modelling of the effectiveness and cost- effectiveness of nonsurgical treatments for women with stress urinary incontinence. Health Technol Assess 14(40)
Sabate E (2003) World Health Organization. Adherence to long term therapies: evidence for action. World Health Organization, Geneva
Van den Bemt JFB, Zwikker HE, van den Ende CHM (2012) Medication adherence in patients with rheumatoid arthritis: a critical appraisal of the existing literature. Expert Rev Clin Immunol 8(4):337–351, http://www.medscape.org/viewarticle/764055 , accessed 14 September 2015
Dumoulin C, Hay-Smith J, Frawley H, McClurg D, Alewijnse D, Bo K et al (2015) 2014 Consensus Statement on Improving Pelvic Floor Muscle Training Adherence: International Continence Society 2011 State-of-the-Science Seminar. Neurourol Urodyn. doi:10.1002/nau.22796
Porta Roda O, Vara Paniagua J, Díaz López MA, Sobrado Lozano P, Simó González M, Díaz Bellido P, Reula Blasco MC, Muñoz GF (2014) Effect of vaginal spheres and pelvic floor muscle training in women with urinary incontinence: a randomized, controlled trial. Neurourol Urodyn. doi:10.1002/nau.22640
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B et al (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J Pelvic Floor Dysfunct 21:5–26
Baden WF, Walker TA (1972) Physical diagnosis in the evaluation of vaginal relaxation. Clin Obstet Gynecol 15(4):1055–1069
Espuña Pons M, Rebollo-Álvarez P, Puig Clota M (2004) Validación de la versión española del International Consultation on Incontinence Questionnaire- Short Form. Un cuestionario para evaluar la incontinencia urinaria. Med Clin (Barc) 122:288–292
Badia Llach X, Castro Diaz D, Conejero Sugranes J (2000) Validity of the King’s Health questionnaire in the assessment of quality of life of patients with urinary incontinence. The King’s Group. Med Clin (Barc) 114:647–652
Márquez E (2004) Métodos de medida del cumplimiento terapéutico en la HTA. Actualizaciones 1:5–6
Hay Smith EJ, Dean S, Burgio K et al (2015) Pelvic-floor-muscle-training adherence ‘Modifiers’: a review of primary qualitative studies—2011 ICS state-of-the-science seminar research paper III of IV. Neurourol Urodyn. doi:10.1002/nau.22771
Bø K, Talseth T (1996) Long-term effect of pelvic floor muscle exercise 5 years after cessation of organized training. Obstet Gynecol 87:261–265
Frawley H, McClurg D, Mahfooza A et al (2015) Health professionals’ and patients’ perspectives on pelvic-floor-muscle-training adherence—2011 ICS state-of-the-science seminar research paper IV of IV. Neurourol Urodyn. doi:10.1002/nau.22774
Bollen JC, Dean SG, Siegert RJ et al (2014) A systematic review of measures of self-reported adherence to unsupervised home-based rehabilitation exercise programmes, and their psychometric properties. BMJ Open 4, e005044. doi:10.1136/bmjopen-2014-005044
Acknowledgments
The authors thank Anna Delgado García and Luisa Varela Sende for data analysis, writing and editing assistance; Carolyn Newey for help with language revision; Ignasi Gich for help with statistical analysis; and Ricard Figueras for help with figures. Funding was received from OPKO Health Spain S.L.U., which also provided the medical device used in the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
This study was selected by the 2015 IUGA Scientific Committee for Oral Poster Presentation (Presentation # OP 110, Control/Tracking Number: 2015-A-781-IUGA) at the 2015 IUGA Meeting in Nice, France (9–13 June 2015).
Rights and permissions
About this article
Cite this article
Porta Roda, O., Díaz López, M.A., Vara Paniagua, J. et al. Adherence to pelvic floor muscle training with or without vaginal spheres in women with urinary incontinence: a secondary analysis from a randomized trial. Int Urogynecol J 27, 1185–1191 (2016). https://doi.org/10.1007/s00192-015-2941-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-015-2941-0