Abstract
Introduction and hypothesis
The aim of this study was to compare robotic or laparoscopic sacrohysteropexy (RLSH) and open sacrohysteropexy (OSH) as a surgical treatment for pelvic organ prolapse (POP).
Methods
Among 111 consecutive patients who had undergone sacrohysteropexy for POP, surgical outcomes and postoperative symptoms were compared between the RLSH (n = 54; robotic 14 cases and laparoscopic 40 cases) and OSH (n = 57). groups The medical records of enrolled patients were reviewed retrospectively.
Results
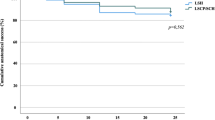
Compared with the OSH group, the RLSH group had shorter operating time (120.2 vs 187.5 min, p < 0.0001), less operative bleeding (median estimated blood loss 50 vs 150 ml; p < 0.0001; mean hemoglobin drop 1.4 vs 2.0 g/dl; p < 0.0001), and fewer postoperative symptoms (13 vs 45.6 %; p < 0.0001). Patients’ overall satisfaction (94.4 vs 91.2 %; p = 0.717) and required reoperation due to postoperative complications (3.7 vs 1.8 %; p = 0.611) did not differ between groups.
Conclusions
RLSH could be a feasible and safe procedure in patients with POP and should be considered as a surgical option that allows preservation of the uterus. Prospective randomized trials will permit the evaluation of potential benefits of RLSH as a minimally invasive surgical approach.

Similar content being viewed by others

References
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89:501–506. doi:10.1016/s0029-7844(97)00058-6
Jelovsek JE, Maher C, Barber MD (2007) Pelvic organ prolapse. Lancet 369:1027–1038. doi:10.1016/s0140-6736(07)60462-0
Dietz HP (2008) The aetiology of prolapse. Int Urogynecol J Pelvic Floor Dysfunct 19:1323–1329. doi:10.1007/s00192-008-0695-7
Mothes AR, Radosa MP, Altendorf-Hofmann A, Runnebaum IB (2015) Risk index for pelvic organ prolapse based on established individual risk factors. Arch Gynecol Obstet. doi:10.1007/s00404-015-3863-2
Thys SD, Roovers JP, Geomini PM, Bongers MY (2012) Do patients prefer a pessary or surgery as primary treatment for pelvic organ prolapse. Gynecol Obstet Investig 74:6–12. doi:10.1159/000336634
Nygaard IE, McCreery R, Brubaker L, Connolly A, Cundiff G, Weber AM, Zyczynski H, Network PFD (2004) Abdominal sacral colpopexy: a comprehensive review. Obstet Gynecol 104:805–823
Ridgeway BM (2015) Does prolapse equal hysterectomy? The role of uterine conservation in women with uterovaginal prolapse. Am J Obstet Gynecol. doi:10.1016/j.ajog.2015.07.035
Korbly NB, Kassis NC, Good MM, Richardson ML, Book NM, Yip S, Saguan D, Gross C, Evans J, Lopes VV, Harvie HS, Sung VW (2013) Patient preferences for uterine preservation and hysterectomy in women with pelvic organ prolapse. Am J Obstet Gynecol 209:470–e1-6. doi:10.1016/j.ajog.2013.08.003
Frick AC, Barber MD, Paraiso MF, Ridgeway B, Jelovsek JE, Walters MD (2013) Attitudes toward hysterectomy in women undergoing evaluation for uterovaginal prolapse. Female Pelvic Med Reconstr Surg 19:103–109. doi:10.1097/SPV.0b013e31827d8667
Barranger E, Fritel X, Pigne A (2003) Abdominal sacrohysteropexy in young women with uterovaginal prolapse: long-term follow-up. Am J Obstet Gynecol 189:1245–1250. doi:10.1067/S0002-9378(03)00665-3
Leron E, Stanton SL (2001) Sacrohysteropexy with synthetic mesh for the management of uterovaginal prolapse. BJOG 108:629–633. doi:10.1111/j.1471-0528.2001.00138.x
Moiety FM, Hegab HM, Ghanem IA, Zedan WM, Salem HA (2010) Abdominal sacrohysteropexy for uterovaginal prolapse: a prospective study on 33 cases. Arch Gynecol Obstet 281:631–636. doi:10.1007/s00404-009-1146-5
Jeon MJ, Jung HJ, Choi HJ, Kim SK, Bai SW (2008) Is hysterectomy or the use of graft necessary for the reconstructive surgery for uterine prolapse? Int Urogynecol J Pelvic Floor Dysfunct 19(3):351–355
Costantini E, Porena M, Lazzeri M, Mearini L, Bini V, Zucchi A (2013) Changes in female sexual function after pelvic organ prolapse repair: role of hysterectomy. Int Urogynecol J 24:1481–1487. doi:10.1007/s00192-012-2041-3
Gutman R, Maher C (2013) Uterine-preserving POP surgery. Int Urogynecol J 24:1803–1813. doi:10.1007/s00192-013-2171-2
Rosati M, Bramante S, Bracale U, Pignata G, Azioni G (2013) Efficacy of laparoscopic sacrocervicopexy for apical support of pelvic organ prolapse. JSLS 17:235–244. doi:10.4293/108680813X13654754535115
Rosati M, Bramante S, Conti F (2014) A review on the role of laparoscopic sacrocervicopexy. Curr Opin Obstet Gynecol 26:281–289. doi:10.1097/GCO.0000000000000079
Li S, Ji M, Zhao Z (2015) The effectiveness of two different laparoscopic surgeries for apical support of pelvic organ prolapse. Eur J Obstet Gynecol Reprod Biol 188:74–78. doi:10.1016/j.ejogrb.2015.03.007
Demirci F, Ozdemir I, Somunkiran A, Topuz S, Iyibozkurt C, Duras Doyran G, Kemik Gul O, Gul B (2007) Perioperative complications in abdominal sacrocolpopexy and vaginal sacrospinous ligament fixation procedures. Int Urogynecol J Pelvic Floor Dysfunct 18:257–261. doi:10.1007/s00192-006-0134-6
Richter HE, Goode PS, Kenton K, Brown MB, Burgio KL, Kreder K, Moalli P, Wright EJ, Weber AM (2007) The effect of age on short-term outcomes after abdominal surgery for pelvic organ prolapse. J Am Geriatr Soc 55:857–863. doi:10.1111/j.1532-5415.2007.01178.x
Germain A, Thibault F, Galifet M, Scherrer ML, Ayav A, Hubert J, Brunaud L, Bresler L (2013) Long-term outcomes after totally robotic sacrocolpopexy for treatment of pelvic organ prolapse. Surg Endosc 27:525–529. doi:10.1007/s00464-012-2472-4
Yoo HN, Kim TJ, Lee YY, Choi CH, Lee JW, Bae DS, Kim BG (2015) Single-site robotic surgery in gynecologic cancer: a pilot study. J Gynecol Oncol 26:62–67. doi:10.3802/jgo.2015.26.1.62
Buchs NC, Pugin F, Ris F, Volonte F, Morel P, Roche B (2013) Early experience with robotic rectopexy. Int J Med Robot 9:e61–e65. doi:10.1002/rcs.1498
Barbash GI, Glied SA (2010) New technology and health care costs--the case of robot-assisted surgery. N Engl J Med 363:701–704. doi:10.1056/NEJMp1006602
Zucchi A, Lazzeri M, Porena M, Mearini L, Costantini E (2010) Uterus preservation in pelvic organ prolapse surgery. Nat Rev Urol 7:626–633. doi:10.1038/nrurol.2010.164
Price N, Slack A, Jackson SR (2010) Laparoscopic hysteropexy: the initial results of a uterine suspension procedure for uterovaginal prolapse. BJOG 117:62–68. doi:10.1111/j.1471-0528.2009.02396.x
van IJsselmuiden MN, Coolen AL, Detollenaere RJ, den Boon J, Bongers M, van de Pol G, Vollebregt A, Radder CM, Deprest J, van Eijndhoven HW (2014) Hysteropexy in the treatment of uterine prolapse stage 2 or higher: a multicenter randomized controlled non-inferiority trial comparing laparoscopic sacrohysteropexy with vaginal sacrospinous hysteropexy (LAVA-trial, study protocol). BMC Womens Health 14:112. doi:10.1186/1472-6874-14-112
Detollenaere RJ, den Boon J, Stekelenburg J, IntHout J, Vierhout ME, Kluivers KB, van Eijndhoven HW (2015) Sacrospinous hysteropexy versus vaginal hysterectomy with suspension of the uterosacral ligaments in women with uterine prolapse stage 2 or higher: multicentre randomised non-inferiority trial. BMJ 351:h3717. doi:10.1136/bmj.h3717
Seror J, Yates DR, Seringe E, Vaessen C, Bitker MO, Chartier-Kastler E, Roupret M (2012) Prospective comparison of short-term functional outcomes obtained after pure laparoscopic and robot-assisted laparoscopic sacrocolpopexy. World J Urol 30:393–398. doi:10.1007/s00345-011-0748-2
Geller EJ, Siddiqui NY, Wu JM, Visco AG (2008) Short-term outcomes of robotic sacrocolpopexy compared with abdominal sacrocolpopexy. Obstet Gynecol 112:1201–1206. doi:10.1097/AOG.0b013e31818ce394
Vitobello D, Siesto G, Bulletti C (2012) Robotic sacral hysteropexy for pelvic organ prolapse. Int J Med Robot 8:114–117. doi:10.1002/rcs.447
Wright JD, Ananth CV, Lewin SN, Burke WM, Lu YS, Neugut AI, Herzog TJ, Hershman DL (2013) Robotically assisted vs laparoscopic hysterectomy among women with benign gynecologic disease. JAMA 309:689–698. doi:10.1001/jama.2013.186
Serati M, Bogani G, Sorice P, Braga A, Torella M, Salvatore S, Uccella S, Cromi A, Ghezzi F (2014) Robot-assisted sacrocolpopexy for pelvic organ prolapse: a systematic review and meta-analysis of comparative studies. Eur Urol 66:303–318. doi:10.1016/j.eururo.2014.02.053
Pan K, Cao L, Ryan NA, Wang Y, Xu H (2015) Laparoscopic sacral hysteropexy versus laparoscopic sacrocolpopexy with hysterectomy for pelvic organ prolapse. Int Urogynecol J. doi:10.1007/s00192-015-2775-9
Siddiqui NY, Grimes CL, Casiano ER, Abed HT, Jeppson PC, Olivera CK, Sanses TV, Steinberg AC, South MM, Balk EM, Sung VW, Society of Gynecologic Surgeons Systematic Review Group (2015) Mesh sacrocolpopexy compared with native tissue vaginal repair: a systematic review and meta-analysis. Obstet Gynecol 125:44–55. doi:10.1097/AOG.0000000000000570
Desille-Gbaguidi H, Hebert T, Paternotte-Villemagne J, Gaborit C, Rush E, Body G (2013) Overall care cost comparison between robotic and laparoscopic surgery for endometrial and cervical cancer. Eur J Obstet Gynecol Reprod Biol 171:348–352. doi:10.1016/j.ejogrb.2013.09.025
Fader AN, Seamon LG, Escobar PF, Frasure HE, Havrilesky LA, Zanotti KM, Secord AA, Boggess JF, Cohn DE, Fowler JM, Skafianos G, Rossi E, Gehrig PA (2012) Minimally invasive surgery versus laparotomy in women with high grade endometrial cancer: a multi-site study performed at high volume cancer centers. Gynecol Oncol 126:180–185. doi:10.1016/j.ygyno.2012.04.028
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Jiheum Paek and Maria Lee contributed equally to this work.
Rights and permissions
About this article
Cite this article
Paek, J., Lee, M., Kim, B.W. et al. Robotic or laparoscopic sacrohysteropexy versus open sacrohysteropexy for uterus preservation in pelvic organ prolapse. Int Urogynecol J 27, 593–599 (2016). https://doi.org/10.1007/s00192-015-2869-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-015-2869-4