Abstract
Introduction and hypothesis
Hormonal contraceptive use is common practice worldwide. Although the effects of hormone treatments in the pelvic region are well established, there is no clear evidence regarding their effects on incontinence, bladder, bowel, vaginal and sexual symptoms in premenopausal women. We hypothesized that hormonal contraceptives affect pelvic floor function. We therefore performed a comprehensive systematic review of published studies to determine the influence of hormonal contraception on pelvic floor functions.
Methods
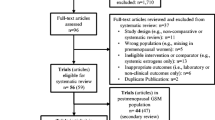
Electronic literature databases were searched from database inception to March 2015. Keywords and medical subject headings searched for included terms and word variations for ‘contraception’, and ‘bowel’, ‘vaginal’, ‘sexual’ and ‘urinary’ symptoms. Studies were eligible if they looked at these symptoms in women taking hormonal contraception. Two reviewers independently screened studies for inclusion, and extracted data on study characteristics, quality and results. Data were combined where possible.
Results
Of the 429 citations identified, 13 studies were included in the review. Data were meta-analysed where possible and presented as prevalence. The results indicate statistically significant links between interstitial cystitis and oral contraceptive use at any point (ever) (OR 2.31, 95 % CI 1.03 – 5.16; p = 0.04) and vulvar vestibulitis and current oral contraceptive use (OR 2.10, 95 % CI 1.26 – 3.49; p = 0.004). The evidence is unclear in other areas.
Conclusions
Our results indicate that oral contraceptives may have an effect on pelvic floor function. They could increase the risk of painful bladder and vulvar vestibulitis, but their effect on dyspareunia is inconsistent. However, robustly collected prospective data to establish causal associations are needed.





Similar content being viewed by others
Abbreviations
- CI:
-
Confidence Interval
- DMPA:
-
Depot medroxyprogesterone acetate
- IC:
-
Interstitial cystitis
- LNG-IUS:
-
Levonorgestrel intrauterine releasing system
- MUI:
-
mixed urinary incontinence
- OAB:
-
Overactive bladder
- OC:
-
Oral contraception/contraceptive
- OR:
-
Odds ratio
- RCT:
-
Randomized controlled trial
- RR:
-
Relative risk
- SUI:
-
Stress urinary incontinence
- UI:
-
Urinary incontinence
References
Hall KS, Trussell J (2012) Types of combined oral contraceptives used by U.S. women. Contraception 86(6):659–665
Iliadou A, Milsom I, Pedersen NL, Altman D (2009) Risk of urinary incontinence symptoms in oral contraceptive users: a national cohort study from the Swedish Twin Register. Fertil Steril 92(2):428–433
Robinson D, Cardozo LD (2003) The role of estrogens in female lower urinary tract dysfunction. Urology 62(4 Suppl 1):45–51
Cody JD, Jacobs ML, Richardson K, Moehrer B, Hextall A (2012) Oestrogen therapy for urinary incontinence in post-menopausal women. Cochrane Database Syst Rev 10:CD001405
O'Halloran T, Bell RJ, Robinson PJ, Davis SR (2012) Urinary incontinence in young nulligravid women: a cross-sectional analysis. Ann Intern Med 157(2):87–93
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151(4):264–269
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJM, Gavaghan DJ (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary. Control Clin Trials 17:1–12
Moher D, Jadad AR, Nichol G, Penman M, Tugwell P, Walsh S (1995) Assessing the quality of randomized controlled trials: an annotated bibliography of scales and checklists. Control Clin Trials 16:62–73
Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M et al (2009) The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. Department of Epidemiology and Community Medicine, University of Ottawa, Canada. http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm
Heliovaara-Peippo S, Halmesmaki K, Hurskainen R, Teperi J, Grenman S, Kivela A et al (2010) The effect of hysterectomy or levonorgestrel-releasing intrauterine system on lower urinary tract symptoms: a 10-year follow-up study of a randomised trial. BJOG 117(5):602–609
Foster DC, Woodruff JD (1995) Case-control study of vulvar vestibulitis syndrome. J Womens Health 4(6):677–680
Townsend MK, Curhan GC, Resnick NM, Grodstein F (2009) Oral contraceptive use and incident urinary incontinence in premenopausal women. J Urol 181(5):2170–2175
Bouchard C, Brisson J, Fortier M, Morin C, Blanchette C (2002) Use of oral contraceptive pills and vulvar vestibulitis: a case-control study. Am J Epidemiol 156(3):254–261
Edgardh K, Abdelnoor M (2007) Vulvar vestibulitis and risk factors: a population-based case-control study in Oslo. Acta Derm Venereol 87(4):350–354
Gardella B, Porru D, Nappi RE, Dacco MD, Chiesa A, Spinillo A (2011) Interstitial cystitis is associated with vulvodynia and sexual dysfunction – a case-control study. J Sex Med 8(6):1726–1734
Warren JW, Clauw DJ, Wesselmann U, Langenberg PW, Howard FM, Morozov V (2011) Sexuality and reproductive risk factors for interstitial cystitis/painful bladder syndrome in women. Urology 77(3):570–575
Burgio KL, Zyczynski H, Locher JL, Richter HE, Redden DT, Wright KC (2003) Urinary Incontinence in the 12-month postpartum period. Obstet Gynecol 102(6):1291–1298
Ekin M, Cengiz H, Ayag ME, Kaya C, Yasar L, Savan K (2013) Effects of the levonorgestrel-releasing intrauterine system on urinary symptoms in patients with adenomyosis. Eur J Obstet Gynecol Reprod Biol 170:517–520
Fraser IS, Dennerstein GJ (1994) Depo-Provera use in an Australian metropolitan practice. Med J Aust 160(9):553–556
Reed BD, Harlow SD, Legocki LJ, Helmuth ME, Haefner HK, Gillespie BW et al (2013) Oral contraceptive use and risk of vulvodynia: a population-based longitudinal study. BJOG 120(13):1678–1684
Smith NK, Jozkowski KN, Sanders SA (2014) Hormonal contraception and female pain, orgasm and sexual pleasure. J Sex Med 11:462–470
Robinson D, Toozs-Hobson P, Cardozo L (2013) The effect of hormones on the lower urinary tract. Menopause 19(4):155–162
Bjorling DE, Wang ZY (2001) Estrogen and neuroinflammation. Urology 57(6 Suppl 1):40–46
Cheng Y, Keast JR (2009) Effects of estrogens and bladder inflammation on mitogen-activated protein kinases in lumboscaral dorsal root ganglia from adult female rats. BMC Neurosci 10:156
Acknowledgments
We thank Derick Yates, Clinical Librarian of Birmingham Women’s Hospital NHS Trust, for carrying out the literature searches on our behalf.
Compliance with ethical standards
ᅟ
Conflicts of interest
None.
Funding
No funding was sought for this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Champaneria, R., D’Andrea, R.M. & Latthe, P.M. Hormonal contraception and pelvic floor function: a systematic review. Int Urogynecol J 27, 709–722 (2016). https://doi.org/10.1007/s00192-015-2833-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-015-2833-3