Abstract
Introduction
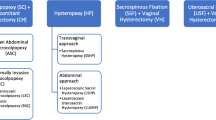
Pelvic organ prolapse is showing an increasing prevalence (3 – 50 %). The gold standard treatment of apical prolapse is sacrocolpopexy which can be performed via minimal access (laparoscopy or robotics) or open approaches. The aim of this review was to appraise the effectiveness of minimal access surgery versus the open approach in the treatment of apical prolapse.
Methods
Keywords were searched in: CINAHL, MEDLINE, CENTRAL, Cochrane MDSG Trials Register, Cochrane Library, Current Controlled Trials, ClinicalTrials.gov, WHO International Trials Registry Platform search portal, LILACS, and Google Scholar databases. Data up to 31 April 2014 were considered. Randomized and nonrandomized controlled trials evaluating all women who underwent minimally invasive sacropexy (MISC) and open sacropexy (OSC) were included. A data extraction tool was used for data collection. MISC was compared with OSC using narrative analysis and meta-analysis (RevMan) where appropriate.
Results
MISC and OSC were compared in 12 studies involving 4,757 participants. MISC and OSC were equally effective in terms of point-C POP-Q measurements and recurrence rate. MISC was associated with a lower transfusion rate (odds ratio 0.41, 95 % CI 0.20 – 0.83), shorter length of hospital stay (mean difference −1.57 days, 95 % CI −1.91 – −1.23 days), and less blood loss (mean difference −113.27 mL, 95 % CI −163.67 – −62.87 mL) but a longer operating time (mean difference 87.47, 95 % CI 58.60 – 116.34, p < 0.0001).
Conclusions
MISC showed similar anatomic results to OSC with a lower transfusion rate, shorter length of hospital stay and less blood loss. The rate of other complications was similar between the approaches. Cautious interpretation of results is advised due to risk of bias caused by the inclusion of nonrandomized studies.













Similar content being viewed by others
References
Barber MD, Maher C (2013) Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J 24(11):1783–1790
Toozs-Hobson P, Kelvin B, Cardozo L (1998) Management of vaginal vault prolapse. Br J Obstet Gynaecol 105:13–17
Turner DA, Shaw C, McGrother CW, Dallosso HM, Cooper NJ (2004) The cost of clinically significant urinary storage symptoms for community dwelling adults in the UK. BJU Int 93(9):1246–1252
Subramanian D, Szwarcensztein K, Mauskopf JA, Slack MC (2009) Rate, type, and cost of pelvic organ prolapse surgery in Germany, France, and England. Eur J Obstet Gynecol Reprod Biol 144(2):177–181
Maher CF, Feiner B, Baessler K, Schmid C (2013) Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev 4:CD004014
Yohannes P, Rotariua P, Pintoa P, Smitha A, Leea B (2002) Comparison of robotic versus laparoscopic skills: is there a difference in the learning curve? Urology 60(1):39–45
Reza M, Maeso S, Blasco JA, Andradas E (2010) Meta-analysis of observational studies on the safety and effectiveness of robotic gynaecological surgery. Br J Surg 97(12):1772–1783
Liu H, Lu D, Wang L, Shi G, Song H, Clarke J (2012) Robotic surgery for benign gynaecological disease. Cochrane Database Syst Rev 2:CD008978
Higgins J, Green S (eds) (2008) Cochrane handbook for systematic reviews of interventions. Wiley-Blackwell, Chichester
Serati M, Bogani G, Sorice P, Braga A, Torella M, Salvatore S et al (2014) Robot-assisted sacrocolpopexy for pelvic organ prolapse: a systematic review and meta-analysis of comparative studies. Eur Urol 66(2):303–318
Petticrew M, Roberts H (2006) Systematic reviews in the social science: a practical guide. Blackwell, Oxford
Nosti PA, Umoh AU, Kane S, White DE, Harvie HS, Lowenstein L et al (2014) Outcomes of abdominal and minimally invasive sacrocolpopexy: a retrospective cohort study. Female Pelvic Med Reconstr Surg 20(1):33–37
Pulliam SJ, Weinstein MM, Wakamatsu MM (2012) Minimally invasive apical sacropexy: a retrospective review of laparoscopic and robotic operating room experiences. Female Pelvic Med Reconstr Surg 18(2):122–126
Ross J, Preston M (2005) Laparoscopic sacrocolpopexy for severe vaginal vault prolapse: five-year outcome. J Minim Invasive Gynecol 12(3):221–226
McGovern DPB, Summerskill WSM, Valori RM, Levi M (2001) Key topics in evidence-based medicine. Bios, Oxford
Weber AM, Abrams P, Brubaker L, Cundiff G, Davis G, Dmochowski RR et al (2001) The standardization of terminology for researchers in female pelvic floor disorders. Int Urogynecol J Pelvic Floor Dysfunct 12:178–186
Cochrane Informatics & Knowledge Management Department (2014) RevMan.
Collins SA, Tulikangas PK, O’Sullivan DM (2012) Effect of surgical approach on physical activity and pain control after sacral colpopexy. Am J Obstet Gynecol 206:438.e1–e6
Geller EJ, Siddiqui NY, Wu JM, Visco AG (2008) Short-term outcomes of robotic sacrocolpopexy compared with abdominal sacrocolpopexy. Obstet Gynecol 112(6):1201–1206
Coolen AWM, van Oudheusden AMJ, van Eijndhoven HWF, van der Heijden TFM, Stokmans RA, Mol BJ, et al. (2013) A comparison of complications between open abdominal sacrocolpopexy and laparoscopic sacrocolpopexy for the treatment of vault prolapse. Obstet Gynecol Int. 2013:528636
Klauschie JL, Suozzi BA, O’Brien MM, McBride AW (2009) A comparison of laparoscopic and abdominal sacral colpopexy: objective outcome and perioperative differences. Int Urogynecol J Pelvic Floor Dysfunct 20(3):273–279
Elliott CS, Hsieh MH, Sokol ER, Comiter CV, Payne CK, Chen B (2012) Robot-assisted versus open sacrocolpopexy: a cost-minimization analysis. J Urol 187(2):638–643
Geller EJ, Parnell BA, Dunivan GC (2012) Robotic vs abdominal sacrocolpopexy: 44-month pelvic floor outcomes. Urology 79(3):532–536
Hoyte L, Rabbanifard R, Mezzich J, Bassaly R, Downes K (2012) Cost analysis of open versus robotic-assisted sacrocolpopexy. Female Pelvic Med Reconstr Surg 18(6):335–339
Khan A, Alperin M, Wu N, Clemens JQ, Dubina E, Pashos CL, Anger JT (2013) Comparative outcomes of open versus laparoscopic sacrocolpopexy among Medicare beneficiaries. Int Urogynecol J 24(11):1883–1891
Tyson MD, Wolter CE (2015) A comparison of 30-day surgical outcomes for minimally invasive and open sacrocolpopexy. Neurourol Urodyn 34(2):151–155
Freeman RM, Pantazis K, Thomson A, Frappell J, Bombieri L, Moran P et al (2013) A randomised controlled trial of abdominal versus laparoscopic sacrocolpopexy for the treatment of post-hysterectomy vaginal vault prolapse: LAS study. Int Urogynecol J 24(3):377–384
Paraiso MFR, Walters M, Rackley R, Melek S, Hugney C (2005) Laparoscopic and abdominal sacral colpopexies: a comparative cohort study. Am J Obstet Gynecol 192:1752–1758
Tyagi V, Hawthorn R, Guerrero K (2013) Sacrocolpopexy (SCP) - A Cohort Study Looking at Short, Medium and Long Term Outcome. Medical & Surgical Urology 2(118).
Barber MD, Maher C (2013) Apical prolapse. Int Urogynecol J 24:1815–1833
Chapron C, Fauconnier A, Goffinet F, Bréart G, Dubuisson JB (2002) Laparoscopic surgery is not inherently dangerous for patients presenting with benign gynaecologic pathology. Results of a meta-analysis. Hum Reprod 17(5):1334–1342
Claerhout F, Roovers JP, Lewi P, Verguts J, De Ridder D, Deprest J (2009) Implementation of laparoscopic sacrocolpopexy – a single centre’s experience. Int Urogynecol J Pelvic Floor Dysfunct 20(9):1119–1125
Medeiros LR, Rosa DD, Bozzetti MC, Fachel JM, Furness S, Garry R, et al. (2009) Laparoscopy versus laparotomy for benign ovarian tumour. Cochrane Database Syst Rev 2:CD004751
de la Orden SG, Reza MM, Blasco JA, Andradas E, Callejo D, Pérez T (2008) Laparoscopic hysterectomy in the treatment of endometrial cancer: a systematic review. J Minim Invasive Gynecol 15(4):395–401
Acknowledgments
We acknowledge the valuable guidance of Andrea De Gouveia De Sa as a research assistant in the development of this paper and the team from Anglia Ruskin University library for their support in the database search and acquisition of the majority of the included papers.
Conflicts of interest
Maribel De Gouveia De Sa: Nothing to disclose
Leica Sarah Claydon: Nothing to disclose
Barry Whitlow: Nothing to disclose
Maria Angelica Dolcet Artahona: Nothing to disclose
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix S1
(DOC 32 kb)
Appendix S2
(DOC 31 kb)
Appendix S3
(DOC 31 kb)
Appendix S4
(DOC 31 kb)
Appendix S5
(DOC 31 kb)
Appendix S6
(DOC 32 kb)
Appendix S7
(DOC 31 kb)
Appendix S8
(DOC 31 kb)
Appendix S9
(DOC 31 kb)
Appendix S10
(DOC 31 kb)
Appendix S11
(DOC 31 kb)
Appendix S12
(DOC 31 kb)
Appendix S13
(DOC 31 kb)
Appendix S14
(DOC 31 kb)
Appendix S15
(DOC 31 kb)
Appendix S16
(DOC 31 kb)
Appendix S17
(DOC 26 kb)
Appendix S18
(DOC 31 kb)
Appendix S19
(DOC 26 kb)
Appendix S20
(DOC 26 kb)
Appendix S21
(DOC 26 kb)
Appendix S22
(DOC 26 kb)
Appendix S23
(DOC 30 kb)
Rights and permissions
About this article
Cite this article
De Gouveia De Sa, M., Claydon, L.S., Whitlow, B. et al. Laparoscopic versus open sacrocolpopexy for treatment of prolapse of the apical segment of the vagina: a systematic review and meta-analysis. Int Urogynecol J 27, 3–17 (2016). https://doi.org/10.1007/s00192-015-2765-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-015-2765-y