Abstract
Introduction and hypothesis
To date, there is no overall consensus on the definition of cure after surgery for pelvic organ prolapse (POP). The aim of the study was to design and test the scoring system S.A.C.S. (Satisfaction–Anatomy–Continence–Safety) to assess and compare the outcomes of POP repair.
Methods
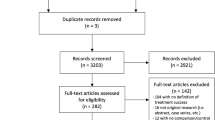
A total of 233 women underwent open sacrocolpopexy. The S.A.C.S. outcome scoring system was scheduled at 24 months of follow-up, and each component was detected according to: Satisfaction by mean of Patient Global Improvement Inventory scale, Anatomy by mean of POP Quantification system and bulge symptom, Continence by mean of pad use, and Safety by mean of the Clavien–Dindo classification of surgical complications. Each component produced a binary nominal categorical variable (1 or 0), with a total score of 4 representing cure. As a comparative tool, patients answered a simple yes/no question: “If you had to undergo surgery all over again, would you still do it?”. The degree of concordance was estimated using Cohen’s Kappa test.
Results
According to the S.A.C.S. scoring system, only 160 patients (68.6 %) reached the maximum score of cure. Sensitivity of the S.A.C.S. score was 74.1 %, specificity was 90 %, total diagnostic capacity was 75.5 %. The S.A.C.S. score internal consistency was good; the k-coefficient was higher for the satisfaction component of the score (k = 0.560).
Conclusion
This study proposes an original, simple post-operative scoring system integrating satisfaction, anatomy, continence, and safety reports for patients undergoing surgery for POP, providing a complete, although perfectible, method to accurately report outcomes in all clinical scenarios.


Similar content being viewed by others
References
Barber MD, Maher C (2013) Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J 24:1783–1790
Wu JM, Matthews CA, Conover MM, Pate V, Jonsson Funk M (2014) Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol 123:1201–1206
Clark AL, Gregory T, Smith VJ, Edwards R (2003) Epidemiologic evaluation of reoperation for surgically treated pelvic organ prolapse and urinary incontinence. Am J Obstet Gynecol 189:1261–1267
Hullfish KL, Bovbjerg VE, Gibson J, Steers WD (2002) Patient-centred goals for pelvic floor dysfunction surgery: what is success, and is it achieved? Am J Obstet Gynecol 187:88–92
Brubaker L, Shull R (2005) EGGS for patient-centred outcomes. Int Urogynecol J Pelvic Floor Dysfunct 16:171–173
Espuña-Pons M, Fillol M, Pascual MA, Rebollo P, Mora AM, Female Pelvic Floor Dysfunction Research Group (Grupo de Investigación en Disfunciones del Suelo Pélvico en la Mujer-GISPEM) (2014) Pelvic floor symptoms and severity of pelvic organ prolapse in women seeking care for pelvic floor problems. Eur J Obstet Gynecol Reprod Biol 177:141–145
Lee U, Raz S (2011) Emerging concepts for pelvic organ prolapse surgery: what is cure? Curr Urol Rep 12:62–67
Artibani W, Pesce F, Prezioso D, Scarpa RM, Zattoni F, Tubaro A, Rizzi CA, Santini AM, Simoni L, FLOW Study Group (2006) Italian validation of the urogenital distress inventory and its application in LUTS patients. Eur Urol 50:1323–1329
Raz S, Erickson DR (1992) SEAPI-QMM incontinence classi¢cation system. Neurourol Urodyn 111:187
Doran, George T (1981) There’s a S.M.A.R.T. way to write management’s goals and objectives. Management Review 70 (11)
Srikrishna S, Robinson D, Cardozo L (2010) Validation of the patient global impression of improvement (PGI-I) for urogenital prolapse. Int Urogynecol J Pelvic Floor Dysfunct 21:523–528
Srikrishna S, Robinson D, Cardozo L (2010) A longitudinal study of patient and surgeon goal achievement 2 years after surgery following pelvic floor dysfunction surgery. BJOG 117:1504–1511
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, Shull BL, Smith AR (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien–Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196
Hosmer DW, Lemeshow S (2000) Applied logistic regression. Wiley, New York
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Cvach K, Dwyer P (2012) Surgical management of pelvic organ prolapse: abdominal and vaginal approaches. World J Urol 30:471–477
Toozs-Hobson P, Freeman R, Barber M, Maher C, Haylen B, Athanasiou S, Swift S, Whitmore K, Ghoniem G, de Ridder D, International Urogynecological Association; International Continence Society (2012) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for reporting outcomes of surgical procedures for pelvic organ prolapse. Neurourol Urodyn 31:415–421
Lee RK, Mottrie A, Payne CK, Waltregny D (2014) A review of the current status of laparoscopic and robot-assisted sacrocolpopexy for pelvic organ prolapse. Eur Urol 65:1128–1137
Serati M, Bogani G, Sorice P, Braga A, Torella M, Salvatore S, Uccella S, Cromi A, Ghezzi F (2014) Robot-assisted sacrocolpopexy for pelvic organ prolapse: a systematic review and meta-analysis of comparative studies. Eur Urol 66:303–318
Barber MD, Brubaker L, Nygaard I, Wheeler TL 2nd, Schaffer J, Chen Z, Spino C (2009) Pelvic floor disorders network: defining success after surgery for pelvic organ prolapse. Obstet Gynecol 114:600–609
Jelovsek JE, Maher C, Barber MD (2007) Pelvic organ prolapse. Lancet 369:1027–1038
Srikrishna S, Robinson D, Cardozo L, Cartwright R (2008) Experiences and expectations of women with urogenital prolapse: a quantitative and qualitative exploration. BJOG 115:1362–1368
Lowenstein L, Fitzgerald MP, Kenton K, Dooley Y, Templehof M, Mueller ER, Brubaker L (2008) Patient-selected goals: the fourth dimension in assessment of pelvic floor disorders. Int Urogynaecol J Pelvic Floor Dysfunct 19:81–84
Robinson D, Anders K, Cardozo L (2003) What do women want? Interpretation of the concept of cure. J Pelvic Med Surg 9:273–277
Baskayne K, Willars J, Pitchforth E, Tincello DG (2014) Women’s expectations of prolapse surgery: a retrospective qualitative study. Neurourol Urodyn 33:85–89
Dietz V, Maher C (2013) Pelvic organ prolapse and sexual function. Int Urogynecol J 24:1853–1857
Filocamo MT, Serati M, Li Marzi V, Costantini E, Milanesi M, Pietropaolo A, Polledro P, Gentile B, Maruccia S, Fornia S, Lauri I, Alei R, Arcangeli P, Sighinolfi MC, Manassero F, Andretta E, Palazzetti A, Bertelli E, Del Popolo G, Villari D (2014) The Female Sexual Function Index (FSFI): linguistic validation of the Italian version. J Sex Med 11:447–453
Lawndy SS, Withagen MI, Kluivers KB, Vierhout ME (2011) Between hope and fear: patient’s expectations prior to pelvic organ prolapse surgery. Int Urogynecol J 22:1159–1163
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mearini, L., Zucchi, A., Nunzi, E. et al. The S.A.C.S. (Satisfaction–Anatomy–Continence–Safety) score for evaluating pelvic organ prolapse surgery: a proposal for an outcome-based scoring system. Int Urogynecol J 26, 1061–1067 (2015). https://doi.org/10.1007/s00192-015-2655-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-015-2655-3