Abstract
Introduction and hypothesis
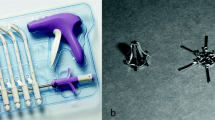
The aim of the study was to compare rates of success, mesh exposure, and surgical re-intervention after trocar-guided Gynemesh PS™ and trocarless Polyform™ transvaginal mesh procedures.
Methods
We conducted a retrospective cohort study of all transvaginal mesh procedures performed at our centers between January 2008 and May 2012. Multiple logistic regression models were used to explore the binary outcomes of objective and subjective success rates, as well as mesh exposure and re-intervention rates, between the two procedures after adjustment for patient’s age, parity, body mass index, smoking status, previous hysterectomy, previous prolapse surgery, and follow-up time.
Results
We included 103 transvaginal mesh procedures (47 trocar-guided Gynemesh PS™ and 56 trocarless Polyform™). In both groups, Pelvic Organ Prolapse Quantification (POP-Q) scores were significantly improved after the procedure. Median follow-up was 340 days and interquartile range (IQR) 152–644. Objective success rates were 55.3 % (26/47) in the trocar group and 60.7 % (34/56) in the trocarless group (p = 0.9), whereas subjective success was 83.0 % (39/47) and 94.6 % (53/56), respectively (p = 0.1). The adjusted odds of developing mesh exposure were significantly less after trocarless transvaginal mesh procedures compared to trocar-guided ones [odds ratio (OR) 0.16, 95 % confidence interval (CI) 0.03–0.97]. Surgical re-interventions, aimed mostly at treating recurrent prolapse, mesh exposure, and latent stress urinary incontinence, were also significantly less frequent after trocarless procedures [5 patients (8.9 %) requiring re-intervention versus 15 (31.9 %), respectively, adjusted OR 0.15, 95 % CI 0.04–0.60].
Conclusions
Trocar-guided Gynemesh PS™ and trocarless Polyform™ transvaginal mesh systems result in similar objective and subjective success rates. The newer Polyform™ mesh results in significantly fewer mesh exposures and surgical re-interventions.
Similar content being viewed by others
References
FDA (2008) FDA Public Health Notification: serious complications associated with transvaginal placement of surgical mesh in repair of pelvic organ prolapse and stress urinary incontinence. http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/PublicHealthNotifications/ucm061976.htm. Accessed 22 Mar 2013
FDA (2011) FDA Safety Communication: update on serious complications associated with transvaginal placement of surgical mesh for pelvic organ prolapse. http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm262435.htm. Accessed 22 Mar 2013
Maher C, Feiner B, Baessler K, Schmid C (2013) Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev 4:CD004014. doi:10.1002/14651858.CD004014.pub5
Vu MK, Letko J, Jirschele K, Gafni-Kane A, Nguyen A, Du H, Goldberg RP (2012) Minimal mesh repair for apical and anterior prolapse: initial anatomical and subjective outcomes. Int Urogynecol J 23(12):1753–1761. doi:10.1007/s00192-012-1780-5
Jones KA, Feola A, Meyn L, Abramowitch SD, Moalli PA (2009) Tensile properties of commonly used prolapse meshes. Int Urogynecol J Pelvic Floor Dysfunct 20(7):847–853. doi:10.1007/s00192-008-0781-x
Shepherd JP, Feola AJ, Abramowitch SD, Moalli PA (2012) Uniaxial biomechanical properties of seven different vaginally implanted meshes for pelvic organ prolapse. Int Urogynecol J 23(5):613–620. doi:10.1007/s00192-011-1616-8
Alcalay M, Cosson M, Livneh M, Lucot JP, Von Theobald P (2011) Trocarless system for mesh attachment in pelvic organ prolapse repair–1-year evaluation. Int Urogynecol J 22(5):551–556. doi:10.1007/s00192-010-1349-0
Moore RD, Mitchell GK, Miklos JR (2012) Single-incision vaginal approach to treat cystocele and vault prolapse with an anterior wall mesh anchored apically to the sacrospinous ligaments. Int Urogynecol J 23(1):85–91. doi:10.1007/s00192-011-1536-7
Lukban JC, Roovers JP, Vandrie DM, Erickson T, Zylstra S, Patel MP, Moore RD (2012) Single-incision apical and posterior mesh repair: 1-year prospective outcomes. Int Urogynecol J 23(10):1413–1419. doi:10.1007/s00192-012-1692-4
Stanford EJ, Moore RD, Roovers JP, Courtieu C, Lukban JC, Bataller E, Liedl B, Sutherland SE (2013) Elevate anterior/apical: 12-month data showing safety and efficacy in surgical treatment of pelvic organ prolapse. Female Pelvic Med Reconstr Surg 19(2):79–83. doi:10.1097/SPV.0b013e318278cc29
Bump RC, Mattiasson A, Bø K, Brubaker LP, DeLancey JO, Klarskov P, Shull BL, Smith AR (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175(1):10–17
Tan JS, Lukacz ES, Menefee SA, Powell CR, Nager CW, San Diego Pelvic Floor Consortium (2005) Predictive value of prolapse symptoms: a large database study. Int Urogynecol J Pelvic Floor Dysfunct 16(3):203–209. doi:10.1007/s00192-004-1243-8, discussion 209
Box GE, Tidwell PW (1962) Transformation of independent variables. Technometrics 4:531–550
Allison PD (1999) Logistic regression using the SAS system: theory and application. SAS Institute, Cary
Hosmer DW, Lemeshow S (2000) Applied logistic regression, 2nd edn. Wiley, Hoboken
Maher CF, Feiner B, DeCuyper EM, Nichlos CJ, Hickey KV, O’Rourke P (2011) Laparoscopic sacral colpopexy versus total vaginal mesh for vaginal vault prolapse: a randomized trial. Am J Obstet Gynecol 204(4):360.e1–360.e7. doi:10.1016/j.ajog.2010.11.016
Altman D, Väyrynen T, Engh ME, Axelsen S, Falconer C, Nordic Transvaginal Mesh Group (2011) Anterior colporrhaphy versus transvaginal mesh for pelvic-organ prolapse. N Engl J Med 364(19):1826–1836. doi:10.1056/NEJMoa1009521
Miller D, Lucente V, Babin E, Beach P, Jones P, Robinson D (2011) Prospective clinical assessment of the transvaginal mesh technique for treatment of pelvic organ prolapse-5-year results. Female Pelvic Med Reconstr Surg 17(3):139–143. doi:10.1097/SPV.0b013e3182175da6
Azaïs H, Charles CJ, Delporte P, Debodinance P (2012) Prolapse repair using the Elevate™ kit: prospective study on 70 patients. Int Urogynecol J 23(10):1421–1428. doi:10.1007/s00192-012-1673-7
Withagen MI, Vierhout ME, Milani AL (2010) Does trocar-guided tension-free vaginal mesh (Prolift) repair provoke prolapse of the unaffected compartments? Int Urogynecol J 21(3):271–278. doi:10.1007/s00192-009-1028-1
Withagen MI, Milani AL, de Leeuw JW, Vierhout ME (2012) Development of de novo prolapse in untreated vaginal compartments after prolapse repair with and without mesh: a secondary analysis of a randomised controlled trial. BJOG 119(3):354–360. doi:10.1111/j.1471-0528.2011.03231.x
De Landsheere L, Ismail S, Lucot JP, Deken V, Foidart JM, Cosson M (2012) Surgical intervention after transvaginal Prolift mesh repair: retrospective single-center study including 524 patients with 3 years’ median follow-up. Am J Obstet Gynecol 206(1):83.e1–83.e7. doi:10.1016/j.ajog.2011.07.040
Ogah J, Cody DJ, Rogerson L (2011) Minimally invasive synthetic suburethral sling operations for stress urinary incontinence in women: a short version Cochrane review. Neurourol Urodyn 30(3):284–291. doi:10.1002/nau.20980
Rehman H, Bezerra CC, Bruschini H, Cody JD (2011) Traditional suburethral sling operations for urinary incontinence in women. Cochrane Database Syst Rev 1:CD001754. doi:10.1002/14651858.CD001754.pub3
Kow N, Goldman HB, Ridgeway B (2013) Management options for women with uterine prolapse interested in uterine preservation. Curr Urol Rep 14(5):395–402. doi:10.1007/s11934-013-0336-7
Zucchi A, Lazzeri M, Porena M, Mearini L, Costantini E (2010) Uterus preservation in pelvic organ prolapse surgery. Nat Rev Urol 7(11):626–633. doi:10.1038/nrurol.2010.164
Acknowledgements
Funding was obtained from the Academic Enrichment Fund of the McGill University Health Center’s Obstetrics and Gynecology Department, Montreal, QC.
Conflicts of interest
Dr. Walter is a consultant for Boston Scientific and Gynecare, Ethicon and has received financial compensation from presentations for Boston Scientific, Gynecare, and Duchesnay. Dr. Merovitz has received financial compensation from a presentation for Duschesnay. Dr. Larouche and Dr. Correa have no financial disclosure.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Larouche, M., Merovitz, L., Correa, J.A. et al. Outcomes of trocar-guided Gynemesh PS™ versus single-incision trocarless Polyform™ transvaginal mesh procedures. Int Urogynecol J 26, 71–77 (2015). https://doi.org/10.1007/s00192-014-2467-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-014-2467-x