Abstract
Introduction and hypothesis
Two-dimensional magnetic resonance imaging (MRI) of posterior vaginal prolapse has been studied. However, the three-dimensional (3-D) mechanisms causing such prolapse remain poorly understood. This discovery project was undertaken to identify the different 3-D characteristics of models of rectocele-type posterior vaginal prolapse (PVPR) in women.
Methods
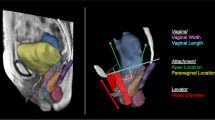
Ten women with (cases) and ten without (controls) PVPR were selected from an ongoing case-control study. Supine, multiplanar MR imaging was performed at rest and maximal Valsalva. Three-dimensional reconstructions of the posterior vaginal wall and pelvic bones were created using 3D Slicer v. 3.4.1. In each slice the posterior vaginal wall and perineal skin were outlined to the anterior margin of the external anal sphincter to include the area of the perineal body. Women with predominant enteroceles or anterior vaginal prolapse were excluded.
Results
The case and control groups had similar demographics. In women with PVPR two characteristics were consistently visible (10/10): (1) the posterior vaginal wall displayed a folding phenomenon similar to a person beginning to kneel (“kneeling” shape) and (2) a downward displacement in the upper two thirds of the vagina. Also seen in some, but not all of the scans were: (3) forward protrusion of the distal vagina (6/10), (4) perineal descent (5/10), and (5) distal widening in the lower third of the vagina (3/10).
Conclusions
Increased folding (kneeling) of the vagina and an overall downward displacement are consistently present in rectocele. Forward protrusion, perineal descent, and distal widening are sometimes seen as well.



Similar content being viewed by others
References
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89(4):501–506
Boyles SH, Weber AM, Meyn L (2003) Procedures for pelvic organ prolapse in the United States, 1979–1997. Am J Obstet Gynecol 188(1):108–115
Silva WA, Pauls RN, Segal JL, Rooney CM, Kleeman SD, Karram MM (2006) Uterosacral ligament vault suspension: five-year outcomes. Obstet Gynecol 108(2):255–263
Subak LL, Waetjen LE, van den Eeden S, Thom DH, Vittinghoff E, Brown JS (2001) Cost of pelvic organ prolapse surgery in the United States. Obstet Gynecol 98(4):646–651
Chen L, Ashton-Miller JA, DeLancey JO (2009) A 3D finite element model of anterior vaginal wall support to evaluate mechanisms underlying cystocele formation. J Biomech 42(10):1371–1377
Larson KA, Hsu Y, Chen L, Ashton-Miller JA, DeLancey JO (2010) Magnetic resonance imaging-based three-dimensional model of anterior vaginal wall position at rest and maximal strain in women with and without prolapse. Int Urogynecol J 21(9):1103–1109
Hsu Y, Chen LY, Summers A, Ashton-Miller JA, DeLancey JOL (2008) Anterior vaginal wall length and degree of anterior compartment prolapse seen on dynamic MRI. Int Urogynecol J Pelvic Floor Dysfunct 19(1):137–142
Ganeshan A, Anderson EM, Upponi S, Planner AC, Slater A, Moore N, D’Costa H, Bungay H (2008) Imaging of obstructed defecation. Clin Radiol 63(1):18–26
Kelvin FM, Maglinte DD, Hale DS, Benson JT (2000) Female pelvic organ prolapse: a comparison of triphasic dynamic MR imaging and triphasic fluoroscopic cystocolpoproctography. AJR Am J Roentgenol 174(1):81–88
Lewicky-Gaupp C, Yousuf A, Larson KA, Fenner DE, Delancey JO (2010) Structural position of the posterior vagina and pelvic floor in women with and without posterior vaginal prolapse. Am J Obstet Gynecol 202(5):497.e1–497.e6
Pannu HK, Scatarige JC, Eng J (2009) Comparison of supine magnetic resonance imaging with and without rectal contrast to fluoroscopic cystocolpoproctography for the diagnosis of pelvic organ prolapse. J Comput Assist Tomogr 33(1):125–130
Larson KA, Luo J, Yousuf A, Ashton-Miller JA, Delancey JO (2012) Measurement of the 3D geometry of the fascial arches in women with a unilateral levator defect and “architectural distortion.” Int Urogynecol J 23(1):57–63
DeLancey JO (1999) Structural anatomy of the posterior pelvic compartment as it relates to rectocele. Am J Obstet Gynecol 180(4):815–823
Hsu Y, Lewicky-Gaupp C, DeLancey JO (2008) Posterior compartment anatomy as seen in magnetic resonance imaging and 3-dimensional reconstruction from asymptomatic nulliparas. Am J Obstet Gynecol 198(6):651.e1–651.e7
Summers A, Winkel LA, Hussain HK, DeLancey JO (2006) The relationship between anterior and apical compartment support. Am J Obstet Gynecol 194(5):1438–1443
Larson KA, Luo J, Guire KE, Chen L, Ashton-Miller JA, DeLancey JO (2012) 3D analysis of cystoceles using magnetic resonance imaging assessing midline, paravaginal, and apical defects. Int Urogynecol J 23(3):285–293
Kleeman SD, Karram M (2008) Posterior pelvic floor prolapse and a review of the anatomy, preoperative testing and surgical management. Minerva Ginecol 60(2):165–182
Paraiso MF, Barber MD, Muir TW, Walters MD (2006) Rectocele repair: a randomized trial of three surgical techniques including graft augmentation. Am J Obstet Gynecol 195(6):1762–1771
Altman D, López A, Kierkegaard J, Zetterström J, Falconer C, Pollack J, Mellgren A (2005) Assessment of posterior vaginal wall prolapse: comparison of physical findings to cystodefecoperitoneography. Int Urogynecol J Pelvic Floor Dysfunct 16(2):96–103, discussion 103
Kenton K, Shott S, Brubaker L (1997) Vaginal topography does not correlate well with visceral position in women with pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct 8(6):336–339
Kenton K, Shott S, Brubaker L (1999) The anatomic and functional variability of rectoceles in women. Int Urogynecol J Pelvic Floor Dysfunct 10(2):96–99
Cundiff GW, Fenner D (2004) Evaluation and treatment of women with rectocele: focus on associated defecatory and sexual dysfunction. Obstet Gynecol 104(6):1403–1421
Acknowledgments
We gratefully acknowledge support from the National Institutes of Health Office for Research on Women’s Health, Specialized Centers of Research on Sex and Gender Factors Affecting Women’s Health, Grant P50 HD 044406.
Conflicts of interest
Dr. John O.L. DeLancey and Dr. James A. Ashton-Miller receive research support from American Medical Systems and Kimberly Clark Corporation. Dr. Ashton-Miller receives research support from Proctor & Gamble, Inc. Dr. DeLancey receives research support from Johnson and Johnson. Dr. Dee E. Fenner receives research support from American Medical Systems. Jiajia Luo’s doctoral studies are partially funded by American Medical Systems and Kimberly Clark Corporation. Dr. Kindra A. Larson has no disclosure to report.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Luo, J., Larson, K.A., Fenner, D.E. et al. Posterior vaginal prolapse shape and position changes at maximal Valsalva seen in 3-D MRI-based models. Int Urogynecol J 23, 1301–1306 (2012). https://doi.org/10.1007/s00192-012-1760-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-012-1760-9