Abstract
Introduction and hypothesis
The aim of the present study was to assess the relationship between lower urinary tract symptoms, anatomical findings, and baseline characteristics in women with pelvic organ prolapse (POP).
Methods
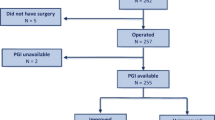
A cross-sectional observational study was performed, enrolling consecutive women seeking cares for lower urinary tract symptoms (LUTS) with evidence of POP. Data regarding baseline characteristics, LUTS, and physical examination were gathered for each patient. Multivariate analysis (multiple linear regression (MLR)) and artificial neural networks (ANNs) were performed to design predicting models.
Results
A total of 1,344 women were included. Age, BMI, pelvic organ prolapse quantification (POP-Q) stage I, and previous surgery for urinary incontinence resulted predictors of urgency and stress incontinence. POP-Q stages III–IV were related to voiding dysfunction and POP symptoms. Age, BMI, and menopausal status resulted predictors for sexual dysfunction. Receiver operating characteristic comparison confirmed that ANNs were more accurate than MLRs in identifying predictors of LUTS.
Conclusions
LUTS result from a fine interaction between baseline characteristics and anatomical findings. ANNs are valuable instrument for better understanding complex biological models.

Similar content being viewed by others
References
Brubaker L, Glazener C, Jacquetin B et al (2008) Surgery for pelvic organ prolapse. Committee 15. In: Abrams P, Cordozo L, Koury S, Wein A (eds) 4th International Consultation on Incontinence. Health Publication Ltd, Paris
Burrows LJ, Meyn LA, Walters MD, Weber AM (2004) Pelvic symptoms in women with pelvic organ prolapse. Obstet Gynecol 104:982–988
Ghetti C, Gregory WT, Edwards SR, Otto LN, Clark AL (2005) Pelvic organ descent and symptoms of pelvic floor disorders. Am J Obstet Gynecol 193:53–57
FitzGerald MP, Janz NK, Wren PA et al (2007) Prolapse severity, symptoms and impact on quality of life among women planning sacrocolpopexy. Int J Gynecol Obstet 98:24–28
Broekhuis SR, Hendriks JCM, Futterer JJ, Vierhout ME, Barentsz JO, Kluivers KB (2010) Perineal descent and patients’ symptoms of anorectal dysfunction, pelvic organ prolapse, and urinary incontinence. Int Urogynecol J 21:721–729
Ellerkmann RM, Cundiff GW, Melick CF, Nihira MA, Leffler K, Bent AE (2001) Correlation of symptoms with location and severity of pelvic organ prolapse. Am J Obstet Gynecol 185:1332–1338
Gutman RE, Ford DE, Quiroz LH, Shippey SH, Handa VL (2008) Is there a pelvic organ prolapse threshold that predicts pelvic floor symptoms? Am J Obstet Gynecol 199:683.e1–683.e7
Washington BB, Erekson EA, Kassis NC, Myers DL (2010) The association between obesity and stage II or greater prolapse. Am J Obstet Gynecol 202(503):e1–e4
Baxt WG (1995) Application of artificial neural network to clinical medicine. Lancet 346:1135–1138
Forsstrom JJ, Dalton KJ (1995) Artificial neural networks for decision support in clinical medicine. Ann Med 27:509–517
Maher C, Feiner B, Baessler K, Adams EJ, Hagen S, Glazener CMA (2010) Surgical management of pelvic organ prolapse in women. Cochrane Database of Systematic Reviews Issue 4. Art. No.: CD004014. doi:10.1002/14651858.CD004014.pub4
Basheer IA, Hajmeer M (2000) Artificial neural networks: fundamentals, computing, design, and application. J Microbiol Methods 43:3–31
Dreiseitl S, Ohno-Machado L (2002) Logistic regression and artificial neural network classification models: a methodology review. J Biomed Inform 35:352–359
Rumelhart DE, Hinton GE, Williams RL (1986) Learning representation by backpropagating errors. Nature 323:533–536
Tu JV (1997) Advantages and disadvantages of using artificial neural networks versus logistic regression for predicting medical outcomes. J Clin Epidemiol 49:1225–1231
Digesu GA, Santamato S, Khullar V et al (2003) Validation of an Italian version of the prolapse quality of life questionnaire. Eur J Obstet Gynecol Reprod Biol 106:184–192
Haylen BT, de Ridder D, Freeman RM et al (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J 21:5–26
Schafer W, Abrams P, Liao L et al (2002) Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn 21:261–274
Abrams P, Andersson KE, Birder L et al (2010) Fourth International Consultation on Incontinence recommendations of the International Scientific Commettee: evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn 29:213–240
Almeida JS (2002) Predictive non-linear modeling of complex data by artificial neural networks. Curr Opin Biotechnol 13:72–76
DeLancey JO, Low LK, Miller JM et al (2008) Graphic integration of causal factors of pelvic floor disorders: an integrated life span model. Am J Obstet Gynecol 199:610–615
Digesu AL, Salvatore S, Fernando R, Khullar V (2008) Mixed urinary symptoms: what are the urodynamic findings? Neurourol Urodyn 27:372–375
Swift SE, Tate SB, Nicholas J (2003) Correlation of symptoms with degree of pelvic organ support in a general population of women: what is pelvic organ prolapse? Am J Obstet Gynecol 189:372–379
Salvatore S, Athanasiou S, Digesu GA et al (2009) Identification of risk factors for genital prolapse recurrence. Neurourol Urodyn 29:301–304
Oliver RL (1980) A cognitive model of the antecedents and consequences of satisfaction decisions. J Mark Res 17:460–469
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Salvatore, S., Serati, M., Siesto, G. et al. Correlation between anatomical findings and symptoms in women with pelvic organ prolapse using an artificial neural network analysis. Int Urogynecol J 22, 453–459 (2011). https://doi.org/10.1007/s00192-010-1300-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-010-1300-4