Abstract
Introduction and hypothesis
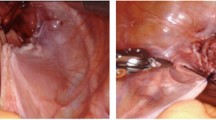
The aim was to assess the efficacy of three-compartment pelvic organ prolapse (POP) vaginal repair using the InteXen® biocompatible porcine dermal graft as compared to traditional colporrhaphy with sacrospinous ligament suspension.
Methods
Preoperative, operative, postoperative and follow-up data were collected retrospectively. Objective recurrence was defined as POP quantification ≥ stage II and subjective recurrence as a symptomatic bulge.
Results
Each group consisted of 63 patients. Surgery time was longer using InteXen® (72 ± 24.5 vs 55 ± 23.5 min, p = 0.0002). Length of hospital stay (4.6 ± 1.6 vs 4.9 ± 2.1 days, p = 0.34) as well as duration of follow-up (37.1 vs 35.7 months, p = 0.45) were equivalent between the two groups. No case of mesh erosion or infection was noted. The objective (17% vs 8%, p = 0.12) and subjective recurrence rates (13% vs 5%, p = 0.12) between the two groups were not statistically different.
Conclusions
InteXen® was well tolerated but had similar efficacy to traditional colporrhaphy and sacrospinous ligament suspension.

Similar content being viewed by others
Abbreviations
- POP:
-
Pelvic organ prolapse
- Xen:
-
Group of patients treated with InteXen®
- Trad:
-
Group of patients treated with traditional colporrhaphy and sacrospinous ligament suspension
- POP-Q:
-
Pelvic organ prolapse quantification
- TOT:
-
Transobturator tape
- BMI:
-
Body mass index
References
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89(4):501–563
Fialkow MF, Newton KM, Lentz GM, Weiss NS (2008) Lifetime risk of surgical management for pelvic organ prolapse or urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 19(3):437–440
Diana M, Zoppe C, Mastrangeli B (2000) Treatment of vaginal vault prolapse with abdominal sacral colpopexy using prolene mesh. Am J Surg 179(2):126–128
Maher C, Baessler K, Glazener CMA, Adams EJ, Hagen S (2006) Surgical management of pelvic organ prolapse in women (Cochrane review). Cochrane Library, issue 2
Julian TM (1996) The efficacy of Marlex mesh in the repair of severe, recurrent vaginal prolapse of the anterior midvaginal wall. Am J Obstet Gynecol 175:1472–1475
Gauruder-Burmester A, Koutouzidou P, Rohne J, Gronewold M, Tunn R (2007) Follow-up after polypropylene mesh repair of anterior and posterior compartments in patients with recurrent prolapse. Int Urogynecol J Pelvic Floor Dysfunct 18(9):1059–1064
David-Montefiore E, Barranger E, Dubernard G, Detchev R, Nizard V, Daraï E (2005) Treatment of genital prolapse by hammock using porcine skin collagen implant (Pelvicol®). Urology 66(6):1314–1318
Daraï E, Coutant C, Rouzier R, Ballester M, David-Montefiore E, Apfelbaum D (2009) Genital prolapse repair using porcine skin implant and bilateral sacrospinous fixation: midterm functional outcome and quality-of-life assessment. Urology 73(2):245–250
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, Shull BL, Smith AR (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Winters JC (2006) Intexen tissue processing and laboratory study. Int Urogynecol J Pelvic Floor Dysfunct 17:S34–S38
Mahdy A, Elmissiry M, Ghoniem G (2008) The outcome of transobturator cystocele repair using biocompatible porcine dermis graft: our experience with 32 cases. Int Urogynecol J Pelvic Floor Dysfunct 19:1647–1652
Gomelsky A, Rudy DC, Dmochowski RR (2004) Porcine dermis interposition graft for repair of high grade anterior compartment defects with or without concomitant pelvic organ prolapse procedures. J Urol 171:1581–1584
Leboeuf L, Miles RA, Kim SS, Gousse AE (2004) Grade 4 cystocele repair using four-defect repair and porcine xenograft acellular matrix (Pelvicol®): outcome measures using SEAPI. Urology 64(2):282–286
Botros SM, Sand PK, Beaumont JL, Abramov Y, Miller JJ, Goldberg RP (2009) Arcus-anchored acellular dermal graft compared to anterior colporrhaphy for stage II cystoceles and beyond. Int Urogynecol J Pelvic Floor Dysfunct 20(10):1265–1271
Meschia M, Pifarotti P, Bernasconi F, Magatti F, Riva D, Kocjancic E (2007) Porcine skin collagen implants to prevent anterior vaginal wall prolapse recurrence: a multicenter, randomized study. J Urol 177(1):192–195
Gandhi S, Goldberg RP, Kwon C, Koduri S, Beaumont JL, Abramov Y, Sand PK (2005) A prospective randomized trial using solvent dehydrated fascia latta for the prevention of recurrent anterior vaginal wall prolapse. Am J Obstet Gynecol 192:1649–1654
Paraiso M, Barber M, Muir T, Walters M (2006) Rectocele repair: a randomized trial of three surgical techniques including graft augmentation. Am J Obstet Gynecol 195:1762–1771
Handel LN, Frenkl TL, Kim YH (2007) Results of cystocele repair: a comparison of traditional anterior colporrhaphy, polypropylene mesh and porcine dermis. J Urol 178:153–156
Hiltunen R, Nieminen K, Takala T, Heiskanen E, Merikari M, Niemi K, Heinonen PK (2007) Low-weight polypropylene mesh for anterior vaginal wall prolapse: a randomized controlled trial. Obstet Gynecol 110(2 Pt 2):455–462
Ganj FA, Ibeanu OA, Bedestani A, Nolan TE, Chesson RR (2009) Complications of transvaginal monofilament polypropylene mesh in pelvic organ prolapse repair. Int Urogynecol J Pelvic Floor Dysfunct 20(8):919–925
Collinet P, Belot F, Debodinance P, Ha Duc E, Lucot JP, Cosson M (2006) Transvaginal mesh technique for pelvic organ prolapse repair: mesh exposure management and risk factors. Int Urogynecol J Pelvic Floor Dysfunct 17:315–320
Cosson M, Debodinance P, Boukerrou M, Chauvet MP, Lobry P, Crépin G, Ego A (2003) Mechanical properties of synthetic implants used in the repair of prolapse and urinary incontinence in women: which is the ideal material? Int Urogynecol J Pelvic Floor Dysfunct 14(3):169–178
Dwyer PL (2006) Evolution of biological and synthetic grafts in reconstructive pelvic surgery. Int Urogynecol J Pelvic Floor Dysfunct 17:S10–S15
Jia X, Glazener C, Mowatt G, MacLennan G, Bain C, Fraser C, Burr J (2008) Efficacy and safety of using mesh or grafts in surgery for anterior and/or posterior vaginal wall prolapse: systematic review and meta-analysis. BJOG 115:1350–1361
Van Raalte HM, Lucente VR, Molden SM, Haaf R, Murphy M (2008) One-year anatomic and quality-of-life outcomes after the Prolift procedure for treatment of post-hysterectomy prolapse. Am J Obstet Gynecol 199(6):694.e1–694.e6
Summers A, Winkel LA, Hussain HK, DeLancey JOL (2006) The relationship between anterior and apical compartment support. Am J Obstet Gynecol 194:1438–1443
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ramanah, R., Mairot, J., Clement, MC. et al. Evaluating the porcine dermis graft InteXen® in three-compartment transvaginal pelvic organ prolapse repair. Int Urogynecol J 21, 1151–1156 (2010). https://doi.org/10.1007/s00192-010-1153-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-010-1153-x