Abstract
Introduction and hypothesis
This study aimed to validate a symptom questionnaire to assess presence and patient bother as related to common pelvic floor disorders.
Methods
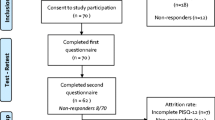
The validation of the Pelvic Floor Bother Questionnaire (PFBQ) included evaluation of internal reliability, test-retest reliability, and validity of the items.
Results
A total of 141 patients with mean age of 61.8 ± 13.2 were included in the study. Twenty-four percent of patients complained of stress urinary incontinence, 14.9% mixed incontinence, 14.9% urge incontinence, 10% fecal incontinence, 5.7% obstructed defecation, 28.4% pelvic organ prolapse, and 2.1% dyspareunia. The PFBQ demonstrated good reliability (α = 0.61-0.74; ICC = 0.94). There was a strong agreement beyond chance observed for each question (k = 0.77-0.91). PFBQ correlated with stage of prolapse (ρ = 0.73, p < 0.0001), number of urinary and fecal incontinence episodes (ρ = 0.81, p < 0.0001; ρ = 0.54, p < 0.0001), and obstructed defecation (ρ = 0.55, p < 0.0001).
Conclusion
The PFBQ is a useful tool that can be easily used for identification and severity or bother assessment of various pelvic floor symptoms.
Similar content being viewed by others
References
Bump RC, Norton PA (1998) Epidemiology and natural history of pelvic floor dysfunction. Obstet Gynecol Clin North Am 25:723–746
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89:501–506
Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, Spino C, Whitehead WE, Wu J, Brody DJ, Pelvic Floor Disorders Network (2008) Prevalence of symptomatic pelvic floor disorders in US women. JAMA 300(11):1311–1316
Jelovsek JE, Maher C, Barber MD (2007) Pelvic organ prolapse. Lancet 369:1027–1038
Jackson SL, Weber AM, Hull TC, Mitchinson AR, Walters MD (1997) Fecal incontinence in women with urinary incontinence and pelvic organ prolapse. Obstet Gynecol 89:423–427
Gonzalez-argente FX, Jain J, Nogueras JJ, Davila GW, Weiss EG, Wexner SD (2001) Prevalence and severity of urinary incontinence and pelvic genital prolapse in females with anal incontinence or rectal prolapse. Dis Colon Rectum 44(7):920–926
Barber MD, Kuchibhatla MN, Pieper CF, Bump RC (2001) Psychometric evaluation of 2 comprehensive condition-specific quality of life instruments for women with pelvic floor disorders. Am J Obstet Gynecol 185:1388–1395
Barber MD, Walters MD, Bump RC (2005) Short forms for two condition-specific quality of life questionnaires for women with pelvic floor disorders (PFDI-20 & PFIQ-7). Am J Obstet Gynecol 193:103
Kelleher CJ, Cardozo LD, Khullar V, Salvatore S (1997) A new questionnaire to assess the quality of life of urinary incontinent women. Br J Obstet Gynaecol 104:1374
Shumaker SA, Wyman JF, Uebersax JS et al (1994) Health-related quality of life measures for women with urinary incontinence: the incontinence impact questionnaire and the urogenital distress inventory. Qual Life Res 3:291
Uebersax JS, Wyman JF, Shumaker SA et al (1995) Short forms to assess life quality and symptom distress for urinary incontinence in women. Neurourol Urodyn 14:131
Jorge JM, Wexner SD (1993) Etiology and management of fecal incontinence. Dis Colon Rectum 36:77
Hull TL, Floruta C, Piedmonte M (2001) Preliminary results of an outcome tool used for evaluation of surgical treatment for fecal incontinence. Dis Colon Rectum 44:799–805
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Abrams P, Cardozo L, Fall M, Griffiths D et al (2003) The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology 61(1):37–49
Walter SD, Eliasziw M, Donner A (1998) Sample size and optimal designs for reliability studies. Stat Med 17:101–110
Acknowledgments
Gabriel P. Suciu, M.S.P.H., Ph.D. for assistance in statistical analysis.
Conflicts of interest
G. Willy Davila: Consultant and speaker: AMS, Watson, Astellas, CL Medical.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix

Rights and permissions
About this article
Cite this article
Peterson, T.V., Karp, D.R., Aguilar, V.C. et al. Validation of a global pelvic floor symptom bother questionnaire. Int Urogynecol J 21, 1129–1135 (2010). https://doi.org/10.1007/s00192-010-1148-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-010-1148-7