Abstract
Introduction and hypothesis
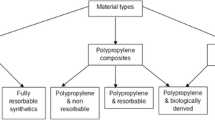
Currently, most implants used for reinforcement in surgical treatment of pelvic floor disorders are knitted monofilament polypropylene (PP). While previously recognized as inert, PP is associated with high complication rates. Some recent literature suggests polyester prosthetics based on poly(ethylene terephthalate) (PET), which may be more inert in vivo.
Methods
A sample of 100 implants explanted from patients due to complications was examined to evaluate the relative degradation characteristics of PP and PET prosthetics. Histological, microscopic (scanning electron microscopy, SEM) and chemical analysis (Fourier transform infrared (FTIR) spectroscopy and differential scanning calorimetry (DSC)) were conducted on these explants.
Results
Poly(ethylene terephtahlate) explants appeared to sustain less degradation in vivo than the PP explants observed in this cohort.
Conclusions
This is the first study to evaluate synthetic implants used in a vaginal approach for pelvic floor reinforcement. The study provides evidence contrary to published literature characterizing PP as inert in such applications. Additionally, the study suggests the need for clinical trials comparatively investigating the performance of new types of monofilament prosthetics, such as those comprising PET.




Similar content being viewed by others
Abbreviations
- PFD:
-
Pelvic floor disorder
- PP:
-
Polypropylene
- PET:
-
Poly(ethylene terephthalate)
- PPMF:
-
Polypropylene monofilament
- LDPPMF:
-
Low density polypropylene monofilament
- HDPPMF:
-
High density polypropylene monofilament
- NKNW:
-
Nonknitted nonwoven polypropylene
- PGA:
-
Poly(glycolic acid)
- FTIR:
-
Fourier transform infrared spectroscopy
- DSC:
-
Differential scanning calorimetry
- SEM:
-
Scanning electron microscopy
References
Culligan PJ, Blackwell L, Goldsmith LJ, Graham CA, Rogers A, Heit MH (2005) A randomized controlled trial comparing fascia lata and synthetic mesh for sacral colpopexy. Obstet Gynecol 106:29–37
Karlovsky ME, Kushner L, Badlani GH (2005) Synthetic biomaterials for pelvic floor reconstruction. Curr Urol Rep 6:376–384
Wu MP (2008) The use of prostheses in pelvic reconstructive surgery: joy or toy? Taiwan J Obstet Gynecol 47:151–156
Debodinance P, Berrocal J, Clave H, Cosson M, Garbin O, Jacquetin B et al (2004) Changing attitudes on the surgical treatment of urogenital prolapse: birth of the tension-free vaginal mesh. J Gynecol Obstet Biol Reprod (Paris) 33:577–588
Bader G, Fauconnier A, Guyot B, Ville Y (2006) Use of prosthetic materials in reconstructive pelvic floor surgery. An evidence-based analysis. Gynecol Obstet Fertil 34:292–297
Caquant F, Collinet P, Debodinance P, Berrocal J, Garbin O, Rosenthal C et al (2008) Safety of trans vaginal mesh procedure: retrospective study of 684 patients. J Obstet Gynaecol Res 34:449–456
Deffieux X, de Tayrac R, Huel C, Bottero J, Gervaise A, Bonnet K et al (2007) Vaginal mesh erosion after transvaginal repair of cystocele using gynemesh or gynemesh-soft in 138 women: a comparative study. Int Urogynecol J Pelvic Floor Dysfunct 18:73–79
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89:501–506
Tsui KP, Ng SC, Tee YT, Yeh GP, Chen GD (2005) Complication of synthetic graft materials used in suburethral sling procedures. Int Urogynecol J Pelvic Floor Dysfunct 16:165–167
Jia X, Glazener C, Mowatt G, MacLennan G, Bain C, Fraser C et al (2008) Efficacy and safety of using mesh or grafts in surgery for anterior and/or posterior vaginal wall prolapse: systematic review and meta-analysis. BJOG 115:1350–1361
Feiner B, Jelovsek JE, Maher C (2009) Efficacy and safety of transvaginal mesh kits in the treatment of prolapse of the vaginal apex: a systematic review. BJOG 116:15–24
Amid PK, Lichtenstein IL (1997) current assessment of lichtenstein tension-free hernia repair. Chirurg 68:959–964
Lefranc O, Bayon Y, Montanari S, Gravagna Ph (in press) Reinforcement materials in Soft Tissue Repair: Key paramaters controlling tolerance and performance-current and future trends in mesh development, in new techniques in genital prolapse surgery.Drs. Theobald P, Zimmerman CW, Davila GW (Eds.)
Caquant F, Collinet P, Deruelle P, Lucot JP, Cosson M (2005) Perineal cellulitis following trans-obturator sub-urethral tape uratape. Eur Urol 47:108–110
Bafghi A, Valerio L, Benizri EI, Trastour C, Benizri EJ, Bongain A (2005) Comparison between monofilament and multifilament polypropylene tapes in urinary incontinence. Eur J Obstet Gynecol Reprod Biol 122:232–236
Martin LK, Yang CQ (1994) Infrared spectroscopy of the photoxidation of a polyethylene nonwoven fabric. J Environ Polym Degrad 2(2):153–159
Clayman HM (1981) Polypropylene. Ophthalmology 88:959–964
Costa L, Jacobson K, Bracco P, Brach del Prever EM (2002) Oxidation of orthopaedic uhmwpe. Biomaterials 23:1613–1624
Bracco P, Brunella V, Trossarelli L, Coda A, Botto-Micca F (2005) Comparison of polypropylene and polyethylene terephthalate (dacron) meshes for abdominal wall hernia repair: a chemical and morphological study. Hernia 9:51–55
Costello CR, Bachman SL, Grant SA, Cleveland DS, Loy TS, Ramshaw BJ (2007) Characterization of heavyweight and lightweight polypropylene prosthetic mesh explants from a single patient. Surg Innov. 14:168–176
Coda A, Bendavid R, Botto-Micca F, Bossoti M, Bona A (2003) Structural alterations of prosthetic meshes in humans. Hernia 7:44–49
Debodinance P, Delporte P, Engrand J, Boulogne M (2002) Development of a better tolerated prosthetic materials: applications in gynecological surgery. J Gynecol Obstet Biol Reprod (Paris) 31:527–540
Altman AJ, Gorn RA, Craft J, Albert DM (1986) The breakdown of polypropylene in the human eye: is it clinically significant? Ann Ophthalmol 18:182–185
Jongebloed WL, Worst JF (1986) Degradation of polypropylene in the human eye: a SEM-study. Doc Ophthalmol 64:143–152
Acknowledgment
Many thanks to Jean-Pierre Laugier for his tremendous pedagogic work with SEM at the CCMA.
Conflicts of interest
The work and research of H. Yahi were supported by a grant from SOFRADIM; S. Montanari is an affiliate of Covidien; Henri Clavé has an educational position for Ethicon Europe.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Clavé, A., Yahi, H., Hammou, JC. et al. Polypropylene as a reinforcement in pelvic surgery is not inert: comparative analysis of 100 explants. Int Urogynecol J 21, 261–270 (2010). https://doi.org/10.1007/s00192-009-1021-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-009-1021-8