Abstract
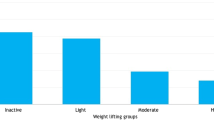
This study describes preoperative physical activity in 314 stress-continent women with prolapse planning sacrocolpopexy. Seventy-six percent reported that they engaged in mild, 60% in moderate, and 26% in strenuous exercise (counts are not mutually exclusive). Activity frequencies did not generally differ by prolapse stage. Prolapse substantially interfered with exercise or recreation in 27% of women, household work or yard work in 19%, and work outside the home in 8%. Compared to women with less symptom distress, more women with greater symptom distress reported that prolapse interfered with household/yard work (43 vs 5%, p<0.0001), working outside the home (29 vs 8%, p<0.005), and recreation/exercise (51 vs 10%, p<0.0001). Prolapse stage was not associated with interference with household/yard work (p=0.28) or work outside home (p=0.89). Although prolapse stage is associated with interference with recreation (p=0.02), this association is not consistently positive : stage II, 42%; stage III, 22%; and stage IV, 32%.

Similar content being viewed by others
References
U.S. Department of Health and Human Services (2000) Healthy people 2010: understanding and improving health, 2nd edn. U.S. Government Printing Office, Washington, DC (November)
Nygaard I, DeLancey JOL, Arnsdorf L, Murphy E (1990) Exercise and incontinence. Obstet Gynecol 75:848–851
Boyles SH, Weber AM, Meyn L (2003) Procedures for pelvic organ prolapse in the United States, 1979–1997. Am J Obstet Gynecol 188:108–115
Samuelsson EC, Victor FTA, Tibblin G, Svardsudd KF (1999) Signs of genital prolapse in a Swedish population of women 20–59 years of age and possible related factors. Am J Obstet Gynecol 180:299–305
Hendrix SL, Clark A, Nygaard I, Aragaki A, Barnabei V, McTiernan A (2002) Pelvic organ prolapse in the Women’s Health Initiative: gravity and gravidity. Am J Obstet Gynecol 186:1160–1166
Brubaker L, Cundiff G, Fine P, Nygaard I, Richter H, Visco A, Zyczynski H, Brown MB, Weber A (2003) A randomized trial of colpopexy and urinary reduction efforts (CARE): design and methods. Control Clin Trials 24:629–642
Brubaker L, Cundiff GW, Fine P, Nygaard I, Richter HE, Visco A, Zyczynski H, Brown MB, Weber AM, for the Pelvic Floor Disorders Network (2006) The CARE Trial: addition of burch colposuspension to abdominal sacrocolpopexy to prevent postoperative urinary stress incontinence. NEJM (in press)
Barber MD, Kuchibhatla M, Pieper CF, Bump RC (2001) Psychometric evaluation of 2 comprehensive condition-specific quality of life instruments for women with pelvic floor disorders. Am J Obstet Gynecol 185:1388–1395
Ware JE Jr, Gandek B (1998) Overview of the SF-36 health survey and the international quality of life assessment (IQOLA) project. J Clin Epidemiol 51:903–912
Bump RC, Mattiasson A, Bo K et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Linn BS, Linn MW, Gurel L (1968) Cumulative illness rating scale. J Am Geriat Soc 16:622–626
Godin G, Shepherd RJ (1985) A simple method to assess exercise behavior in the community. Can J Appl Sport Sci 10:141–146
Hullfish KL, Bovbjerg VE, Gibson J, Steers WD (2002) Patient-centered goals for pelvic floor dysfunction surgery: what is success, and is it achieved? Am J Obstet Gynecol 187:88–92
Acknowledgements
This study was supported by grants from the National Institute of Child Health and Human Development (U01 HD41249, U10 HD41268, U10 HD41248, U10 HD41250, U10 HD41261, U10 HD41263, U10 HD41269, and U10 HD41267).
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
for the Pelvic Floor Disorders Network., Nygaard, I., Handa, V. et al. Physical activity in women planning sacrocolpopexy. Int Urogynecol J 18, 33–37 (2007). https://doi.org/10.1007/s00192-006-0116-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-006-0116-8