Abstract
Purpose
To investigate the aseptic survival of 1.5-stage exchange arthroplasty for periprosthetic joint infection (PJI) after total knee arthroplasty (TKA).
Methods
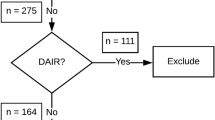
Eighty-eight cases of 1.5-stage exchange arthroplasty for PJI without reinfection were retrospectively analysed. The autoclaved femoral component and new polyethylene insert (PE) were implanted using antibiotic mixed cement. The explanted tibial component was not reinserted. The Western Ontario and McMaster Universities Osteoarthritis Index and range of motion were clinically evaluated preoperatively and at the last follow-up (the last time for the implant in situ). Radiographically, hip–knee–ankle angle (HKA) and component positions were measured preoperatively, postoperatively (1 month after the 1.5-stage exchange arthroplasty), and at the last follow-up. The survival rate was analysed using the Kaplan–Meier method, in which failure was defined as reoperation due to aseptic failure. Mean period to failure and failure site were analysed. Factors affecting survival were investigated in terms of demographics and inappropriateness of the postoperative HKA (HKA > 0 ± 3°) and component positions (α angle > 95 ± 3°, β angle > 90 ± 3°, γ angle > 3 ± 3°, and δ angle > 87 ± 3°).
Results
The spacer in-situ time was 3.7 years (0.2–6.4). The clinical results improved hip–knee–ankle significantly at the last follow-up. Radiographically, the average HKA was valgus 0.1° postoperatively. The average α, β, γ, and δ angles of the postoperative component positions were 95.9°, 90.4°, 3.8°, and 86.7°, respectively. The 1-, 2-, and 5-year postoperative survival rates were 90.9%, 86.4%, and 80.6%, respectively. The mean period to failure was 2.0 years (0.2–5.3). There were 18 cases of aseptic loosening (20.8%), occurring on both the femur and tibial sides in 1 knee, and only on the tibial side in 17 knees. Inappropriate coronal position of the PE (β angle > 90 ± 3°) was a significant factor affecting survival (odds ratio = 5.491; p = 0.011).
Conclusion
The aseptic survival of the 1.5-stage exchange arthroplasty was acceptable when using an autoclaved femoral component and new PE. The appropriate coronal position of the PE helps ensure favourable survival of 1.5-stage exchange arthroplasty.
Level of evidence
IV




Similar content being viewed by others
Data availability
Our data are available in the fgashare repository (https://figshare.com/articles/dataset/1_5_stage_revision_data/24032145).
References
Belay ES, Wixted CM, Kim BI, Wellman SS, Jiranek WA, Bolognesi MP et al (2023) A permanent articulating spacer versus two-stage exchange for chronic periprosthetic joint infection: a propensity score-matched study. J Arthroplasty 38(8):1584–1590
Cho JH, Choi JY, Lee SS (2022) Accuracy of the tibial component alignment by extramedullary system using simple radiographic references in total knee arthroplasty. Medicina (Kaunas) 58(9):1212
Engh GA, Ammeen DJ (1999) Bone loss with revision total knee arthroplasty: defect classification and alternatives for reconstruction. Instr Course Lect 48:167–175
Fleischman AN, Azboy I, Fuery M, Restrepo C, Shao H, Parvizi J (2017) Effect of stem size and fixation method on mechanical failure after revision total knee arthroplasty. J Arthroplasty 32:S202-S208 e201
Goltz DE, Sutter EG, Bolognesi MP, Wellman SS (2018) Outcomes of articulating spacers with autoclaved femoral components in total knee arthroplasty infection. J Arthroplasty 33:2595–2604
Gromov K, Korchi M, Thomsen MG, Husted H, Troelsen A (2014) What is the optimal alignment of the tibial and femoral components in knee arthroplasty? Acta Orthop 85:480–487
Hernandez NM, Buchanan MW, Seyler TM, Wellman SS, Seidelman J, Jiranek WA (2021) 1.5-Stage exchange arthroplasty for total knee arthroplasty periprosthetic joint infections. J Arthroplasty 36:1114–1119
Hoshino T, Watanabe T, Nakagawa Y, Katagiri H, Ozeki N, Ohara T et al (2021) Clinical outcomes of two-stage revision total knee arthroplasty in infected cases with antibiotic-loaded cement spacers produced using a handmade silicone mold. Knee Surg Relat Res 33:27
Indelli PF, Iannotti F, Ferretti A, Valtanen R, Prati P, Perez Prieto D et al (2022) Recommendations for periprosthetic joint infections (PJI) prevention: the European knee associates (EKA)-international committee American association of hip and knee surgeons (AAHKS)-Arthroplasty Society in Asia (ASIA) survey of members. Knee Surg Sports Traumatol Arthrosc 30:3932–3943
Kim CW, Lee CR, Park DH, Kim DY, Kim JW (2021) Clinical outcomes of two-stage revision for chronic periprosthetic joint infection of the knee: culture-negative versus culture-positive. Knee Surg Relat Res 33:28
Kim YH, Park JW, Kim JS, Park SD (2014) The relationship between the survival of total knee arthroplasty and postoperative coronal, sagittal and rotational alignment of knee prosthesis. Int Orthop 38:379–385
Koh YG, Hong HT, Lee HY, Kim HJ, Kang KT (2021) Influence of variation in sagittal placement of the femoral component after cruciate-retaining total knee arthroplasty. J Knee Surg 34:444–451
Koh YG, Lee JA, Lee HY, Suh DS, Park JH, Kang KT (2022) Finite element analysis of femoral component sagittal alignment in mobile-bearing total knee arthroplasty. Biomed Mater Eng 33:195–207
Lee BS, Cho HI, Bin SI, Kim JM, Jo BK (2018) Femoral component varus malposition is associated with tibial aseptic loosening after TKA. Clin Orthop Relat Res 476:400–407
Li P, Zhu Z, Tang X, Shi Z (2022) A mid-term follow-up study on the reimplantation of autoclaved femoral and tibial components as spacers for treating infected total knee arthroplasty. Orthop Surg 14:2042–2049
Liu HX, Shang P, Ying XZ, Zhang Y (2016) Shorter survival rate in varus-aligned knees after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24:2663–2671
Nabet A, Sax OC, Shanoada R, Conway JD, Mont MA, Delanois RE et al (2022) Survival and outcomes of 1.5-stage vs 2-stage exchange total knee arthroplasty following prosthetic joint infection. J Arthroplasty 37:936–941
Parvizi J, Tan TL, Goswami K, Higuera C, Della Valle C, Chen AF et al (2018) The 2018 definition of periprosthetic hip and knee infection: an evidence-based and validated criteria. J Arthroplasty 33(1309–1314):e1302
Parvizi J, Zmistowski B, Berbari EF, Bauer TW, Springer BD, Della Valle CJ et al (2011) New definition for periprosthetic joint infection: from the workgroup of the musculoskeletal infection society. Clin Orthop Relat Res 469:2992–2994
Petis SM, Perry KI, Pagnano MW, Berry DJ, Hanssen AD, Abdel MP (2017) Retained antibiotic spacers after total hip and knee arthroplasty resections: high complication rates. J Arthroplasty 32:3510–3518
Reddy NVR, Saini MK, Reddy PJ, Thakur AS, Reddy CD (2022) Analysis of clinical and radiological outcomes of long tibial stemmed total knee arthroplasty in knee osteoarthritis complicated by tibial stress fracture. Knee Surg Relat Res 34:7
Seo JG, Moon YW, Park SH, Kang HM, Kim SM (2012) How precise is the identification of the center of the femoral head during total knee arthroplasty? Acta Orthop 83:53–58
Siddiqi A, Nace J, George NE, Buxbaum EJ, Ong AC, Orozco FR et al (2019) Primary total knee arthroplasty implants as functional prosthetic spacers for definitive management of periprosthetic joint infection: a multicenter study. J Arthroplasty 34:3040–3047
Song SJ, Le HW, Bae DK, Park CH (2022) Long-term survival of fully cemented stem in re-revision total knee arthroplasty performed on femur with diaphyseal deformation due to implant loosening. Int Orthop 46:1521–1527
Song SJ, Lee HW, Bae DK, Park CH (2020) High incidence of tibial component loosening after total knee arthroplasty using ceramic titanium-nitride-coated mobile bearing prosthesis in moderate to severe varus deformity: a matched-pair study between ceramic-coated mobile bearing and fixed bearing prostheses. J Arthroplasty 35:1003–1008
Song SJ, Lee HW, Kim KI, Park CH (2021) Appropriate determination of the surgical transepicondylar axis can be achieved following distal femur resection in navigation-assisted total knee arthroplasty. Knee Surg Relat Res 33:41
Song SJ, Lee HW, Park CH (2020) A current prosthesis with a 1-mm thickness increment for polyethylene insert could result in fewer adjustments of posterior tibial slope in cruciate-retaining total knee arthroplasty. J Arthroplasty 35(11):3172–3179
Song SJ, Lee HW, Park CH (2022) Medial proximal tibial resorption after total knee arthroplasty according to the design of the cobalt chrome tibial baseplate. Arch Orthop Trauma Surg 143(6):3401–3407
Song SJ, Lee JW, Bae DK, Park CH (2022) Long-term outcomes were similar between hybrid and cemented TKAs performed on paired knees at a minimum 15 years of follow-up. Knee Surg Sports Traumatol Arthrosc 30:832–841
Spinarelli A, Bizzoca D, Moretti L, Vicenti G, Garofalo R, Moretti B (2022) The autoclaving and re-implantation of an infected prosthesis as a spacer during resection knee arthroplasty: a systematic review. Musculoskelet Surg 106:111–125
Tang J, Wu T, Shao H, Zhou Y (2022) Malposition of components and femorotibial mechanical axis changes on pressure distribution in total knee arthroplasty. Clin Biomech (Bristol, Avon) 96:105659
Thakrar RR, Horriat S, Kayani B, Haddad FS (2019) Indications for a single-stage exchange arthroplasty for chronic prosthetic joint infection a systematic review. Bone Joint J. https://doi.org/10.1302/0301-620X.101B1.BJJ-2018-0374.R1
Tsukeoka T, Lee TH, Tsuneizumi Y, Suzuki M (2014) The tibial crest as a practical useful landmark in total knee arthroplasty. Knee 21:283–289
Yoo JH, Chang CB, Shin KS, Seong SC, Kim TK (2008) Anatomical references to assess the posterior tibial slope in total knee arthroplasty: a comparison of 5 anatomical axes. J Arthroplasty 23:586–592
Funding
No external funding was used for this retrospective study.
Author information
Authors and Affiliations
Contributions
The following authors have made substantial contributions to the followings: (1) the conception and design of the study (SJS and CHP), provision of study materials or patients (SJS and CHP), acquisition of data (SHH, HJB and CHP), analysis and interpretation of data (All authors). (2) drafting the article (All authors), (3) final approval of the version to be submitted (All authors).
Corresponding author
Ethics declarations
Conflict of interest
All authors have received no benefits in any form from a commercial party related directly or indirectly to the subject of this article.
Ethical approva
The study was approved by the institutional review boards of our institutions.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Song, S.J., Hwang, S.H., Baek, H.J. et al. Aseptic survival of the 1.5-stage exchange arthroplasty for periprosthetic joint infection was acceptable when using an autoclaved femoral component and a new polyethylene insert. Knee Surg Sports Traumatol Arthrosc 31, 4996–5004 (2023). https://doi.org/10.1007/s00167-023-07552-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-023-07552-3