Abstract
Purpose
The purpose of this study was to compare the incidence of revision in those with pes planovalgus deformity to those without using a large national database. Given the reciprocal changes in lower extremity alignment associated with planovalgus foot deformity, it has been suggested that patients with this deformity has worse outcomes following total knee arthroplasty (TKA).
Methods
A retrospective cohort analysis of patients undergoing elective TKA was conducted using the PearlDiver database. Patients were stratified into three cohorts: those without pes planovalgus, patients with ipsilateral or bilateral pes planovalgus relative to the TKA, and patients with contralateral pes planovalgus. Patients with prior foot reconstructive surgery were excluded. The cohorts were each matched to those without pes planovalgus. Bivariate analysis was performed comparing 90-day medical complications and 2- and 4-year revisions following TKA. An adjusted number needed to be exposed for one additional person to be harmed (NNEH) was calculated using the adjusted odds ratio (OR) and unexposed event rate.
Results
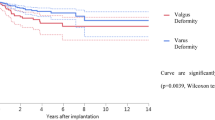
Following matched analysis, those with contralateral pes planovalgus had similar odds (OR 3.41; 95% CI 0.93–12.54; p = n.s.) for aseptic revision within 2 years but significantly higher odds (OR 3.35; 95% CI 1.08–10.41; p = 0.03) within 4 years when compared to those without a pes planovalgus deformity. Within 4 years, there was no significant difference in the incidence of aseptic revision (p = n.s.) in patients with ipsilateral/bilateral pes planovalgus. No patients in any cohort underwent septic revision within 4 years of TKA.
Conclusion
This study found that patients with contralateral pes planovalgus deformity had higher odds of aseptic revision within 4 years following primary TKA in a national database, suggesting that the change in gait kinematics associated with this deformity could possibly be associated with increased revision rates.
Level of evidence
Level III.



Similar content being viewed by others
Abbreviations
- CCI:
-
Charlson comorbidity index
- CI:
-
Confidence interval
- CPT:
-
Current procedural terminology
- ICD:
-
International classification of diseases
- IRB:
-
Institutional review board
- NNEH:
-
Number needed to be exposed for one additional person to be harmed
- OR:
-
Odds ratio
- TKA:
-
Total knee arthroplasty
References
Abdel MP, Bonadurer GF, Jennings MT, Hanssen AD (2015) Increased aseptic tibial failures in patients with a BMI ≥35 and well-aligned total knee arthroplasties. J Arthroplasty 30(12):2181–2184
Aenumulapalli A, Kulkarni MM, Gandotra AR (2017) Prevalence of flexible flat foot in adults: a cross-sectional study. J Clin Diagn Res 11(6):AC17–AC20
Bender R, Blettner M (2002) Calculating the “number needed to be exposed” with adjustment for confounding variables in epidemiological studies. J Clin Epidemiol 55(5):525–530
Burssens A, De Roos D, Barg A, Welck MJ, Krahenbuhl N, Saltzman CL, Victor J (2021) Alignment of the hindfoot in total knee arthroplasty: a systematic review of clinical and radiological outcomes. Bone Joint J 103(1):87–97
Butler JJ, Mercer NP, Hurley ET, Azam MT, Kennedy JG (2021) Alignment of the hindfoot following total knee arthroplasty: a systematic review. World J Orthop 12(10):791–801
Cho WS, Cho HS, Byun SE (2017) Changes in hindfoot alignment after total knee arthroplasty in knee osteoarthritic patients with varus deformity. Knee Surg Sports Traumatol Arthrosc 25(11):3596–3604
Coughlin MJMR (1999) Surgery of the foot and ankle. Mosby, St. Louis, MO
Delanois RE, Mistry JB, Gwam CU, Mohamed NS, Choksi US, Mont MA (2017) Current epidemiology of revision total knee arthroplasty in the United States. J Arthroplasty 32(9):2663–2668
D’Lima DD, Hermida JC, Chen PC, Colwell CW (2001) Polyethylene wear and variations in knee kinematics. Clin Orthop Relat Res 392(392):124–130
Hernigou P, Deschamps G (2004) Alignment influences wear in the knee after medial unicompartmental arthroplasty. Clin Orthop Relat Res 423(423):161–165
Jasper LL, Jones CA, Mollins J, Pohar SL, Beaupre LA (2016) Risk factors for revision of total knee arthroplasty: a scoping review. BMC Musculoskelet Disord. https://doi.org/10.1186/S12891-016-1025-8
Kim YH, Park JW, Jang YS, Kim EJ (2023) Is highly cross-linked polyethylene safe for use in high-flexion posterior stabilized total knee arthroplasty? J Arthroplasty. https://doi.org/10.1016/J.ARTH.2022.08.025
Kodithuwakku Arachchige SNK, Chander H, Knight A (2019) Flat feet: biomechanical implications, assessment and management. Foot 38:81–85
Lauterbach S, Kostev K, Becker R (2010) Characteristics of diabetic patients visiting a podiatry practice in Germany. J Wound Care 19(4):140–148
Meding JB, Keating EM, Ritter MA, Faris PM, Berend ME, Malinzak RA (2005) The planovalgus foot: a harbinger of failure of posterior cruciate-retaining total knee replacement. J Bone Joint Surg 87(12 II SUPPL):59–62
Mullaji A, Shetty GM (2011) Persistent hindfoot valgus causes lateral deviation of weightbearing axis after total knee arthroplasty. Clin Orthop Relat Res 469(4):1154–1160
Petersen KK, Simonsen O, Laursen MB, Nielsen TA, Rasmussen S, Arendt-Nielsen L (2015) Chronic postoperative pain after primary and revision total knee arthroplasty. Clin J Pain 31(1):1–6
Richie D (2020) Biomechanics and orthotic treatment of the adult acquired flatfoot. Clin Podiatr Med Surg 37(1):71–89
Sharkey PF, Lichstein PM, Shen C, Tokarski AT, Parvizi J (2014) Why are total knee arthroplasties failing today–has anything changed after 10 years? J Arthroplasty 29(9):1774–1778
Siddiqi A, Mont MA, Krebs VE, Piuzzi NS (2021) Not All robotic-assisted total knee arthroplasty are the same. J Am Acad Orthop Surg 29(2):45–59
Srivastava A, Lee GY, Steklov N, Colwell CW, Ezzet KA, D’Lima DD (2012) Effect of tibial component varus on wear in total knee arthroplasty. Knee 19(5):560–563
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
ZCP: conception, design, data acquisition and analysis, interpretation of data, drafting original manuscript, and revising manuscript; ABH: conception, design, interpretation of data, and revising manuscript; ARA: conception, design, data acquisition and analysis, interpretation of data, drafting original manuscript, and revising manuscript; RTK: interpretation of data, drafting original manuscript, and revising manuscript; JM: conception and drafting original manuscript; UA: conception and revising manuscript; GJG: interpretation of data and revising manuscript SCT: interpretation of data and revising manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Zachary Pearson, Andrew Harris, Amil Agarwal, R. Timothy Kreulen, Jalen Martin, and Uzoma Ahiarakwe declare that they have no conflict of interest. Gregory Golladay reports leadership roles with AAOS, the Virginia Orthopaedic Society, and the Journal of Arthroplasty and royalties from Stryker and Arthroplasty Today. Savyasachi Thakkar reports leadership roles with AAOS, Arthroplasty Today, and the Journal of Arthroplasty and unpaid consultant work with OrthoAlign and KCL.
Ethical approval
Our institution’s IRB judged this study to be exempt from IRB review.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pearson, Z.C., Harris, A.B., Agarwal, A.R. et al. Higher revision rates in patients with preoperative contralateral pes planovalgus deformity following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 31, 4920–4926 (2023). https://doi.org/10.1007/s00167-023-07520-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-023-07520-x