Abstract
Purpose
Though an increasing number of adults older than 50 years are undergoing hip arthroscopy for treatment of Femoroacetabular Impingement Syndrome (FAIS), it is unclear how their timeline for functional outcome improvement compares to that of younger patients. The purpose of this study was to assess the impact of age on time to achieving the Minimum Clinically Important Difference (MCID), Substantial Clinical Benefit (SCB), and Patient Acceptable Symptom State (PASS) following primary hip arthroscopy for FAIS.
Methods
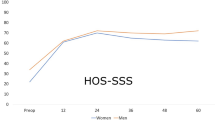
A retrospective comparative single-surgeon cohort study of primary hip arthroscopy patients with minimum 2-year follow-up was conducted. Age categories were 20–34 years, 35–49 years, and 50–75 years. All subjects completed the modified Harris Hip Score (mHHS) prior to surgery and at 6-month, 1-year, and 2-year follow-up. MCID and SCB cutoffs were defined as pre-to-postoperative increases in mHHS by ≥ 8.2 and ≥ 19.8, respectively. PASS cutoff was set at postoperative mHHS ≥ 74. Time to achievement of each milestone was compared using interval-censored survival analysis. The effect of age was adjusted for Body Mass Index (BMI), sex, and labral repair technique using an interval-censored proportional hazards model.
Results
Two hundred eighty-five patients were included in the analysis with 115 (40.4%) aged 20–34 years, 92 (32.3%) aged 35–49 years, and 78 (27.4%) aged 50–75 years. There were no significant differences between groups in time to achievement for the MCID (n.s.) or SCB (n.s.). However, patients in the oldest group had significantly longer time to PASS than those in the youngest group, both in the unadjusted analysis (p = 0.02) and after adjusting for BMI, sex, and labral repair technique (HR 0.68, 95% CI 0.48–0.96, p = 0.03).
Conclusion
Achievement of the PASS, but not the MCID or SCB, is delayed among FAIS patients aged 50–75 years who undergo primary hip arthroscopy compared to those aged 20–34 years. Older FAIS patients should be counseled appropriately about their longer timeline to achieving hip function comparable to their younger counterparts.
Level of evidence
III.


Similar content being viewed by others
Data availability
Data not available due to privacy restrictions.
References
Beck EC, Drager J, Nwachukwu BU, Jan K, Rasio J, Nho SJ (2021) Gender and age-specific differences observed in rates of achieving meaningful clinical outcomes 5-years after hip arthroscopy for femoroacetabular impingement syndrome. Arthroscopy 37:2488.e2481-2496.e2481
Bloom DA, Buchalter D, Kirby DJ, Wang C, Driesman AS, Youm T (2021) Males achieve similar success at two years following hip arthroscopy irrespective of age. Bull Hosp Jt Dis (2013) 79:152–157
Bloom DA, Fried JW, Bi AS, Kaplan DJ, Chintalapudi N, Youm T (2020) Age-associated pathology and functional outcomes after hip arthroscopy in female patients: analysis with 2-year follow-up. Am J Sports Med 48:3265–3271
Bonazza NA, Homcha B, Liu G, Leslie DL, Dhawan A (2018) Surgical trends in arthroscopic hip surgery using a large national database. Arthroscopy 34:1825–1830
Chahal J, Van Thiel GS, Mather RC 3rd, Lee S, Song SH, Davis AM et al (2015) The patient acceptable symptomatic state for the modified Harris hip score and hip outcome score among patients undergoing surgical treatment for femoroacetabular impingement. Am J Sports Med 43:1844–1849
Cvetanovich GL, Weber AE, Kuhns BD, Alter J, Harris JD, Mather RC 3rd et al (2018) Hip arthroscopic surgery for femoroacetabular impingement with capsular management: factors associated with achieving clinically significant outcomes. Am J Sports Med 46:288–296
Domb BG, Linder D, Finley Z, Botser IB, Chen A, Williamson J et al (2015) Outcomes of hip arthroscopy in patients aged 50 years or older compared with a matched-pair control of patients aged 30 years or younger. Arthroscopy 31:231–238
Frank RM, Lee S, Bush-Joseph CA, Salata MJ, Mather RC 3rd, Nho SJ (2016) Outcomes for hip arthroscopy according to sex and age: a comparative matched-group analysis. J Bone Jt Surg Am 98:797–804
Huang HJ, Dang HH, Mamtimin M, Yang G, Zhang X, Wang JQ (2022) Hip Arthroscopy for femoroacetabular impingement syndrome shows good outcomes and low revision rates, with young age and low postoperative pain score predicting excellent five-year outcomes. Arthroscopy. https://doi.org/10.1016/j.arthro.2022.03.024
Lee WY, Kang C, Hwang DS, Jeon JH, Zheng L (2016) Descriptive epidemiology of symptomatic femoroacetabular impingement in young athlete: single center study. Hip Pelvis 28:29–34
Lin LJ, Akpinar B, Bloom DA, Youm T (2021) Age and outcomes in hip arthroscopy for femoroacetabular impingement: a comparison across 3 age groups. Am J Sports Med 49:82–89
Maldonado DR, Kyin C, Shapira J, Rosinsky PJ, Meghpara MB, Ankem HK et al (2021) Defining the maximum outcome improvement of the modified Harris hip score, the nonarthritic hip score, the visual analog scale for pain, and the international hip outcome tool-12 in the arthroscopic management for femoroacetabular impingement syndrome and labral tear. Arthroscopy 37:1477–1485
Montgomery SR, Ngo SS, Hobson T, Nguyen S, Alluri R, Wang JC et al (2013) Trends and demographics in hip arthroscopy in the United States. Arthroscopy 29:661–665
Nwachukwu BU, Chang B, Adjei J, Schairer WW, Ranawat AS, Kelly BT et al (2018) Time required to achieve minimal clinically important difference and substantial clinical benefit after arthroscopic treatment of femoroacetabular impingement. Am J Sports Med 46:2601–2606
Nwachukwu BU, Chang B, Fields K, Rebolledo BJ, Nawabi DH, Kelly BT et al (2017) Defining the “Substantial Clinical Benefit” after arthroscopic treatment of femoroacetabular impingement. Am J Sports Med 45:1297–1303
Nwachukwu BU, Fields K, Chang B, Nawabi DH, Kelly BT, Ranawat AS (2017) Preoperative outcome scores are predictive of achieving the minimal clinically important difference after arthroscopic treatment of femoroacetabular impingement. Am J Sports Med 45:612–619
Ouyang VW, Saks BR, Maldonado DR, Jimenez AE, Ankem HK, Sabetian PW et al (2022) Younger age, capsular repair, and larger preoperative alpha angles are associated with earlier achievement of clinically meaningful improvement after hip arthroscopy for femoroacetabular impingement syndrome. Arthroscopy 38:2195–2203
Schairer WW, Nwachukwu BU, McCormick F, Lyman S, Mayman D (2016) Use of hip arthroscopy and risk of conversion to total hip arthroplasty: a population-based analysis. Arthroscopy 32:587–593
Sing DC, Feeley BT, Tay B, Vail TP, Zhang AL (2015) Age-related trends in hip arthroscopy: a large cross-sectional analysis. Arthroscopy 31:2307.e2302-2313.e2302
Wolfson TS, Ryan MK, Begly JP, Youm T (2019) Outcome trends after hip arthroscopy for femoroacetabular impingement: when do patients improve? Arthroscopy 35:3261–3270
Zusmanovich M, Haselman W, Serrano B, Banffy M (2022) The incidence of hip arthroscopy in patients with femoroacetabular impingement syndrome and labral pathology increased by 85% between 2011 and 2018 in the United States. Arthroscopy 38:82–87
Funding
No funding was received for this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Thomas Youm has received speaker fees, consulting fees, and intellectual property royalties from Arthrex, Inc. The remaining authors have no conflicts of interest to declare.
Ethical approval
New York University School of Medicine, Office of Science and Research Institutional Review Board, New York, NY, USA, Approval #20-01686.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shankar, D.S., Rao, N., Colasanti, C.A. et al. Patients aged 50–75 years take longer to achieve the patient acceptable symptom state than patients aged 20–34 years following primary hip arthroscopy for femoroacetabular impingement syndrome. Knee Surg Sports Traumatol Arthrosc 31, 4510–4518 (2023). https://doi.org/10.1007/s00167-023-07478-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-023-07478-w