Abstract
Purpose
To describe the proximity of the neurovascular structures surrounding the adductor magnus (ADM), to delineate a safe boundary focusing on the techniques used during graft harvest and to evaluate whether the length of the ADM tendon is sufficient for safe medial patellofemoral ligament (MPFL) reconstruction.
Methods
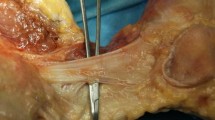
Sixteen formalin-fixed cadavers were dissected. The area surrounding the ADM, the adductor tubercle (AT) and the adductor hiatus was exposed. The following measurements were performed: the (1) total length of MPFL, (2) distance between the AT and the saphenous nerve, (3) the point where the saphenous nerve pierces the vasto-adductor membrane, (4) the point where the saphenous nerve crosses the ADM tendon, (5) the musculotendinous junction of the ADM tendon, and (6) the point where the vascular structures exit the adductor hiatus. Additionally, (7) the distance between the ADM musculotendinous junction and the nearest vessel (popliteal artery), (8) the distance between the ADM (at the level where the saphenous nerve crosses) and the nearest vessel, (9) the length between the AT and the superior medial genicular artery, and finally (10) the depth between the AT and the superior medial genicular artery were analyzed.
Results
The in situ length of the native MPFL was 47.6 ± 42.2 mm. The saphenous nerve pierces the vasto-adductor membrane at a mean distance of 100 mm, although it crosses the ADM itself at an average of 67.6 mm. The vascular structures, on the other hand, become vulnerable at a distance of 89.1 ± 114.0 mm from the AT. After harvesting the ADM tendon, the mean length was found to be 46.9 mm, which was insufficient for fixation. Partial release from the AT resulted in a more adequate length for fixation (65.4 ± 88.7 mm).
Conclusion
The adductor magnus tendon is a viable option for the dynamic reconstruction of the MPFL. Knowledge of the surrounding busy neurovascular topography is paramount for a procedure typically performed in a minimally invasive way. The study results are clinically relevant, as they suggest that tendons should be shorter than the minimum distance from the nerve. If in some cases the length of the MPFL is longer than the distance of the ADM from the nerve, the results suggest that a partial dissection of the anatomical structures might be needed. Direct visualization of the harvesting region might be considered in such cases.




Similar content being viewed by others
Data availability
This article containts no additional data for publications. Any additional data will be presented upon request.
References
Cregar WM, Huddleston HP, Wong SE, Farr J, Yanke AB (2022) Inconsistencies in reporting risk factors for medial patellofemoral ligament reconstruction failure: a systematic review. Am J Sports Med 50:867–877
Dandu N, Trasolini NA, Hevesi M, Zavras AG, Elias TJ, Haneberg EC et al (2022) Landmarks used in medial patellofemoral ligament reconstruction have variable topography. Arthrosc Sports Med Rehabil 4:e2043–e2050
Fırat A, Veizi E, Çepni Ş, Subaşı İÖ, Kılıçarslan K (2020) The “motionless gastrocnemius”: a reliable sign for safe graft harvesting. Arthrosc Tech 9:e1879–e1884
García Hernández JM, López-Vidriero Tejedor E, Castañeda González S, Yrayzoz Fuentes J, Periáñez Moreno R, Saval Benítez JM et al (2022) Posterior hamstring harvest improves aesthetic satisfaction and decreases sensory complications as compared to the classic anterior approach in anterior cruciate ligament reconstruction surgery. J Exp Orthop 9:109. https://doi.org/10.1186/s40634-022-00547-y
Migliorini F, Pilone M, Eschweiler J, Marsilio E, Hildebrand F, Maffulli N (2022) High rates of damage to the medial patellofemoral ligament, lateral trochlea, and patellar crest after acute patellar dislocation: magnetic resonance imaging analysis. Arthroscopy 38:2472–2479
Milinkovic DD, Fink C, Kittl C, Sillanpaa P, Herbst E, Raschke MJ et al (2021) Anatomic and biomechanical properties of flat medial patellofemoral ligament reconstruction using an adductor magnus tendon graft: a human cadaveric study. Am J Sports Med 49:1827–1838
Perea SH, Shannon SR, Green DW (2022) Medial patellofemoral ligament reconstruction with open physes. Clin Sports Med 41:97–108
Perez-Prieto D, Capurro B, Gelber PE, Ginovart G, Reina F, Sanchis-Alfonso V et al (2017) The anatomy and isometry of a quasi-anatomical reconstruction of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc 25:2420–2423
Pilone C, Bonasia DE, Rosso F, Cottino U, Mazzola C, Blonna D et al (2019) Medial patellofemoral ligament reconstruction and nonanatomic stabilization techniques in skeletally immature patients. Joints 7:98–106
Rueth MJ, Koehl P, Schuh A, Goyal T, Wagner D (2023) Return to sports and short-term follow-up of 101 cases of medial patellofemoral ligament reconstruction using gracilis tendon autograft in children and adolescents. Arch Orthop Trauma Surg 143:447–452
Ruffilli A, De Fine M, Traina F, Pilla F, Fenga D, Faldini C (2017) Saphenous nerve injury during hamstring tendons harvest: Does the incision matter? A systematic review. Knee Surg Sports Traumatol Arthrosc 25:3140–3145
Shamrock AG, Day MA, Duchman KR, Glass N, Westermann RW (2019) Medial patellofemoral ligament reconstruction in skeletally immature patients: a systematic review and meta-analysis. Orthop J Sports Med 7:2325967119855023
Tsubosaka M, Matsushita T, Kuroda R, Matsumoto T, Kurosaka M (2017) Pseudoaneurysm of the articular branch of the descending genicular artery following double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 25:2721–2724
Vellios EE, Trivellas M, Arshi A, Beck JJ (2020) Recurrent patellofemoral instability in the pediatric patient: management and pitfalls. Curr Rev Musculoskelet Med 13:58–68
Walker M, Maini L, Kay J, Siddiqui A, Almasri M, de Sa D (2022) Femoral tunnel malposition is the most common indication for revision medial patellofemoral ligament reconstruction with promising early outcomes following revision reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc 30:1352–1361
Xu J, Ye Z, Qiao Y, Xu C, Han K, Chen J et al (2022) Medial patellofemoral ligament reconstruction using adductor-transfer and adductor-sling at nonanatomic femoral attachment sites leads to unfavorable graft-length change patterns: a descriptive biomechanical study. Arthroscopy 38:1557–1567
Zhang YQ, Zhang Z, Wu M, Zhou YD, Tao SL, Yang YL et al (2022) Medial patellofemoral ligament reconstruction: a review. Medicine (Baltimore) 101:e28511. https://doi.org/10.1097/MD.0000000000028511
Funding
The authors did not and will not receive any funding for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no conflicts of interest regarding this study.
Ethical approval
The study design was approved by our local ethics committee.
Informed consent
N/A.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Güngör, Y., Veizi, E., Yılmaz, M. et al. The adductor magnus tendon is a viable option for medial patellofemoral ligament reconstruction, but with a busy surrounding neurovascular topography. Knee Surg Sports Traumatol Arthrosc 31, 4000–4006 (2023). https://doi.org/10.1007/s00167-023-07451-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-023-07451-7