Abstract
Purpose
To investigate the radiographic and clinical outcomes of non-surgical treatment for medial meniscus posterior root tear (MMPRT), and prognostic factors for osteoarthritis (OA) progression and clinical failure.
Methods
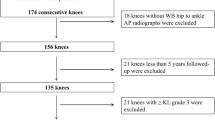
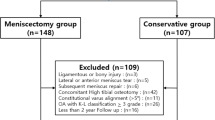
A prospectively collected database was retrospectively reviewed for patients who were diagnosed with acute medial meniscus posterior root tear (MMPRT) between 2013 and 2021 and treated non-surgically for more than 2 years. Patient demographic characteristics and clinical outcomes including pain numeric rating scale (NRS), International Knee Documentation Committee (IKDC) subjective score, Lysholm score, and Tegner activity scale were evaluated. For radiographic evaluation, knee radiographs were obtained to assess the angle of knee alignment and Kellgren–Lawrence (K–L) grade during the first and annually follow-up visits. Baseline magnetic resonance (MR) images were reviewed for the presence of medial meniscus extrusion, bone marrow edema, subchondral insufficiency fracture of medial femoral condyle, and cartilage lesion. The OA progression group was defined as patients who experienced a worsening of one or more grades in the K–L classification system. Prognostic factors were evaluated for OA progression and conversion to total knee arthroplasty (TKA).
Results
Ninety-four patients (90 female and 4 male) with a mean age of 67.0 ± 7.3 years (range, 53–83 years) were followed for a mean of 46.1 ± 22.1 months (range, 24.1–170.5). During the follow-up period, no significant differences in clinical scores were observed, and there were also no significant differences between the groups with and without OA progression. Overall, 12 patients (13%) underwent TKA at a mean of 20.7 ± 16.5 months (range, 8–69 months) and 34 patients (36%) demonstrated OA progression at a mean time of 24 ± 15 months (range, 12–62). The subchondral insufficiency fracture was a prognostic factor for OA progression (p = 0.045 for knee radiograph and p = 0.019 for MR) and conversion to TKA (RR, 4.08 [95% CI 1.23–13.57]; p = 0.022).
Conclusions
Non-surgical treatment for acute medial meniscus posterior root tear did not result in any significant change in clinical outcomes from the initial to the final follow-up. The rate of conversion to arthroplasty was 13%, and the rate of osteoarthritis progression was 36%. Furthermore, subchondral insufficiency fracture was found to be a concomitant prognostic factor correlated with OA progression and conversion to arthroplasty. This information can provide insights for physicians when discussing treatment options with patients, particularly regarding the use of non-surgical treatment and may contribute as a source for future studies of medial meniscus posterior root tear.
Level of evidence
IV.




Similar content being viewed by others
Data availability statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Ahn JH, Jeong HJ, Lee YS, Park JH, Lee JW, Park JH et al (2015) Comparison between conservative treatment and arthroscopic pull-out repair of the medial meniscus root tear and analysis of prognostic factors for the determination of repair indication. Arch Orthop Trauma Surg 135:1265–1276
Bernard CD, Kennedy NI, Tagliero AJ, Camp CL, Saris DBF, Levy BA et al (2020) Medial meniscus posterior root tear treatment: a matched cohort comparison of nonoperative management, partial meniscectomy, and repair. Am J Sports Med 48:128–132
Briggs KK, Kocher MS, Rodkey WG, Steadman JR (2006) Reliability, validity, and responsiveness of the Lysholm knee score and Tegner activity scale for patients with meniscal injury of the knee. J Bone Joint Surg Am 88:698–705
Chang PS, Radtke L, Ward P, Brophy RH (2022) Midterm outcomes of posterior medial meniscus root tear repair: a systematic review. Am J Sports Med 50:545–553
Chung KS, Ha JK, Ra HJ, Yu WJ, Kim JG (2020) Root repair versus partial meniscectomy for medial meniscus posterior root tears: comparison of long-term survivorship and clinical outcomes at minimum 10-year follow-up. Am J Sports Med 48:1937–1944
Dirim Mete B, Cilengir AH, Gursoy M, Dag F, Bulut T (2023) Meniscal extrusion, cartilage, bone, and ligament lesions associated with medial meniscus posterior root tear gap. Eur J Radiol 162:110801
Eseonu KC, Neale J, Lyons A, Kluzek S (2022) Are outcomes of acute meniscus root tear repair better than debridement or nonoperative management? A systematic review. Am J Sports Med 50:3130–3139
Han SB, Shetty GM, Lee DH, Chae DJ, Seo SS, Wang KH et al (2010) Unfavorable results of partial meniscectomy for complete posterior medial meniscus root tear with early osteoarthritis: a 5- to 8-year follow-up study. Arthroscopy 26:1326–1332
Hunter DJ, Guermazi A, Lo GH, Grainger AJ, Conaghan PG, Boudreau RM et al (2011) Evolution of semi-quantitative whole joint assessment of knee OA: MOAKS (MRI Osteoarthritis Knee Score). Osteoarthritis Cartilage 19:990–1002
Irrgang JJ, Anderson AF, Boland AL, Harner CD, Neyret P, Richmond JC et al (2006) Responsiveness of the international knee documentation committee subjective knee form. Am J Sports Med 34:1567–1573
Jo C, Hwang D, Ko S, Yang MH, Lee MC, Han HS et al (2022) Deep learning-based landmark recognition and angle measurement of full-leg plain radiographs can be adopted to assess lower extremity alignment. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-07124-x
Kawada K, Furumatsu T, Tamura M, Xue H, Higashihara N, Kintaka K et al (2023) Medial joint space narrowing progresses after pullout repair of medial meniscus posterior root tear. Int Orthop. https://doi.org/10.1007/s00264-023-05701-4
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502
Krivicich LM, Kunze KN, Parvaresh KC, Jan K, DeVinney A, Vadhera A et al (2022) Comparison of long-term radiographic outcomes and rate and time for conversion to total knee arthroplasty between repair and meniscectomy for medial meniscus posterior root tears: a systematic review and meta-analysis. Am J Sports Med 50:2023–2031
Krych AJ, Johnson NR, Mohan R, Dahm DL, Levy BA, Stuart MJ (2018) Partial meniscectomy provides no benefit for symptomatic degenerative medial meniscus posterior root tears. Knee Surg Sports Traumatol Arthrosc 26:1117–1122
Krych AJ, Reardon PJ, Johnson NR, Mohan R, Peter L, Levy BA et al (2017) Non-operative management of medial meniscus posterior horn root tears is associated with worsening arthritis and poor clinical outcome at 5-year follow-up. Knee Surg Sports Traumatol Arthrosc 25:383–389
Kwak YH, Lee S, Lee MC, Han HS (2018) Large meniscus extrusion ratio is a poor prognostic factor of conservative treatment for medial meniscus posterior root tear. Knee Surg Sports Traumatol Arthrosc 26:781–786
LaPrade CM, Foad A, Smith SD, Turnbull TL, Dornan GJ, Engebretsen L et al (2015) Biomechanical consequences of a nonanatomic posterior medial meniscal root repair. Am J Sports Med 43:912–920
Lee JK, Jung M, Yang JH, Song SY, Shin YS, Cha M et al (2020) Repair versus nonrepair of medial meniscus posterior root tear: a systematic review of patients’ selection criteria, including clinical and radiographic outcomes. Medicine (Baltimore) 99:e19499
Lee NH, Seo HY, Sung MJ, Na BR, Song EK, Seon JK (2021) Does meniscectomy have any advantage over conservative treatment in middle-aged patients with degenerative medial meniscus posterior root tear? BMC Musculoskelet Disord 22:742
Neogi DS, Kumar A, Rijal L, Yadav CS, Jaiman A, Nag HL (2013) Role of nonoperative treatment in managing degenerative tears of the medial meniscus posterior root. J Orthop Traumatol 14:193–199
Okazaki Y, Furumatsu T, Kajiki Y, Hiranaka T, Kintaka K, Kodama Y et al (2022) A posterior shiny-corner lesion of the tibia is observed in the early phase after medial meniscus posterior root tear. Eur J Orthop Surg Traumatol 32:301–306
Sayyid S, Younan Y, Sharma G, Singer A, Morrison W, Zoga A et al (2019) Subchondral insufficiency fracture of the knee: grading, risk factors, and outcome. Skeletal Radiol 48:1961–1974
Sonin AH, Pensy RA, Mulligan ME, Hatem S (2002) Grading articular cartilage of the knee using fast spin-echo proton density-weighted MR imaging without fat suppression. AJR Am J Roentgenol 179:1159–1166
Teichtahl AJ, Cicuttini FM, Abram F, Wang Y, Pelletier JP, Dodin P et al (2017) Meniscal extrusion and bone marrow lesions are associated with incident and progressive knee osteoarthritis. Osteoarthritis Cartilage 25:1076–1083
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
We have included four authors, who contributed significantly to this study. Each of the authors has read and concurs with the content in the final manuscript. BSC contributed to methodology, data curation, formal analysis, investigation, visualization, writing—original draft, and writing—review and editing. JHC contributed to data curation, formal analysis, investigation, and writing—review and editing. JPK contributed to data curation, formal analysis, investigation, writing—review and editing. HSH contributed to conceptualization, methodology, project administration, resources, supervision, validation, and writing—review and editing.
Corresponding author
Ethics declarations
Conflict of interest
All authors have no competing interests to declare.
Ethical approval
This study was approved by Seoul National University College of Medicine/Seoul National University Hospital Institutional Review Board. All investigations were conducted in conformity with ethical principles of research.
Informed consent
This study is a retrospective study; then, we were exempted informed consent by the institutional review board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Choi, B.S., Chung, J., Kwak, J. et al. Subchondral insufficiency fracture is a predictive factor of osteoarthritis progression and conversion to arthroplasty in non-surgically treated medial meniscus root tear. Knee Surg Sports Traumatol Arthrosc 31, 4492–4500 (2023). https://doi.org/10.1007/s00167-023-07444-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-023-07444-6