Abstract
Purpose
This international survey aimed to evaluate the potential controversies regarding the management of first patellar dislocation amongst experienced knee surgeries in the treatment of the first episode of patellar dislocation without osteochondral fragments.
Methods
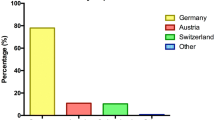
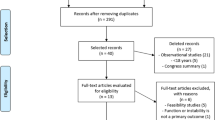
An online survey was conducted from February 2021 to December 2021 to assess the global trend in the diagnosis and management of first-time patellar dislocation without osteochondral fragments. The online survey was accessible on the homepage of the website of the European Society of Sports Traumatology, Knee Surgery and Arthroscopy (ESSKA). The questionnaire consisted of multiple-choice questions and was divided into three sections. The first section consisted of eight questions regarding demographic information, professional activity, and responder experience. The second section consisted of 13 questions regarding the approach to a first patellar dislocation (clinical examination, imaging, and rehabilitation). The third section contained 2 questions concerning the relevance of patient characteristics to the therapeutic algorithm (age, sports, and pathoanatomical predisposing risk factors).
Results
A total of 438 orthopaedic surgeons worldwide completed the questionnaire. At the first approach to diagnose a first-time patellar dislocation, 251 (57%) of the surgeons requested plain radiographs, and 158 (36%) requested magnetic resonance imaging (MRI). In conservatively treated patients, 368 (84%) of the respondents recommended the use of a knee brace. Amongst them, 14 (3%) advocated its use for one week, 75 (17%) for two weeks, 123 (28%) for three weeks, 105 (24%) for four weeks, and 97 (22%) for six weeks. In conservatively treated patients, 215 (49%) of the surgeons recommended load to tolerance, 148 (34%) recommended 30% to 60% of the bodyweight, and 75 (17%) advised against weight-bearing. More than half of the surgeons considered a patient aged less than 35 years practising contact sports to be a candidate for the medial patello-femoral ligament (MPFL) procedure. In addition, a tibial tuberosity to trochlear groove distance (TT-TG) distance of 15 to > 20 mm (for > 75% of the surgeons) and a trochlea types C and D (for > 70% of the surgeons) were considered possible indications for direct surgical management.
Conclusion
At the first approach to diagnose a first-time patellar dislocation, plain radiographs and MRI should be performed. In conservatively treated patients, most of the surgeons recommend weight-bearing to tolerance and a knee brace during the first four weeks, with range of motion of full extension to 30° during the first 15 days and up to 60° for an additional 15 days. Surgical management should be performed in patients in the second and third decades of life practising contact sports and in those patients who present types C and D trochlea dysplasia and patella alta.
Level of evidence
IV.





Similar content being viewed by others
Data availability
The raw data are available upon request to the corresponding author.
References
Cohen D, Le N, Zakharia A, Blackman B, de Sa D (2022) MPFL reconstruction results in lower redislocation rates and higher functional outcomes than rehabilitation: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 30:3784–3795
D’Ambrosi R, Meena A, Raj A, Ursino N, Hewett TE (2022) Anterior knee pain: state of the art. Sports Med Open 8:98
Fu Z, Zhu Z, Chen H, Zhang S (2020) Surgical treatment is better than nonsurgical treatment for primary patellar dislocation: a meta-analysis of randomised controlled trials. Arch Orthop Trauma Surg 140:219–229
Geraghty L, Zordan R, Walker P, Chao TW, Talbot S (2022) Patellar dislocation is associated with increased tibial but not femoral rotational asymmetry. Knee Surg Sports Traumatol Arthrosc 30:2342–2351
Huntington LS, Webster KE, Devitt BM, Scanlon JP, Feller JA (2020) Factors associated with an increased risk of recurrence after a first-time patellar dislocation: a systematic review and meta-analysis. Am J Sports Med 48:2552–2562
Koshino Y, Taniguchi S, Kobayashi T, Samukawa M, Inoue M (2022) Protocols of rehabilitation and return to sport, and clinical outcomes after medial patellofemoral ligament reconstruction with and without tibial tuberosity osteotomy: a systematic review. Int Orthop 46:2517–2528
Liebensteiner M, Keiler A, El Attal R, Balcarek P, Dirisamer F, Giesinger J, Seitlinger G, Nelitz M, Keshmiri A, Frings J, Becher C, Kappel P, Wagner D, Pagenstert G (2021) Conservative versus tailored surgical treatment in patients with first time lateral patella dislocation: a randomized-controlled trial. J Orthop Surg Res 16:378
Ling DI, Brady JM, Arendt E, Tompkins M, Agel J, Askenberger M, Balcarek P, Parikh S, Shubin Stein BE (2021) Development of a multivariable model based on individual risk factors for recurrent lateral patellar dislocation. J Bone Joint Surg Am 103:586–592
Liu JN, Steinhaus ME, Kalbian IL, Post WR, Green DW, Strickland SM, Shubin Stein BE (2018) Patellar instability management: a survey of the international patellofemoral study group. Am J Sports Med 46:3299–3306
Martinez-Cano JP, Chica J, Martinez-Arboleda JJ, Rincón-Escobar E, Zamudio-Castilla L, Renjifo M, Martinez-Rondanelli A (2021) Patellofemoral dislocation recurrence after a first episode: a case-control study. Orthop J Sports Med 9:2325967120981636
Migliorini F, Driessen A, Quack V, Gatz M, Tingart M, Eschweiler J (2020) Surgical versus conservative treatment for first patellofemoral dislocations: a meta-analysis of clinical trials. Eur J Orthop Surg Traumatol 30:771–780
Migliorini F, Pilone M, Eschweiler J, Marsilio E, Hildebrand F, Maffulli N (2022) High rates of damage to the medial patellofemoral ligament, lateral trochlea, and patellar crest after acute patellar dislocation: magnetic resonance imaging analysis. Arthroscopy 38:2472–2479
Milinkovic DD, Jovandic I, Zimmermann F, Balcarek P (2022) The J-sign and the body mass index determine the disease-specific quality of life in patients with lateral patellar instability. Knee Surg Sports Traumatol Arthrosc 30:1672–1678
Musielak BJ, Premakumaran P, Janusz P, Dziurda M, Koch A, Walczak M (2021) Good outcomes of modified Grammont and Langenskiöld technique in children with habitual patellar dislocation. Knee Surg Sports Traumatol Arthrosc 29:1983–1989
Ng J, Broomfield J, Barbosa F, Bhangoo N, Geutjens G (2022) Low re-dislocation rate following Bereiter trochleoplasty for recurrent patellar instability with severe trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-07201-1
Parikh SN, Veerkamp M, Redler LH, Schlechter J, Williams BA, Yaniv M, Friel N, Perea SH, Shannon SR, Green DW (2022) Patellar instability in young athletes. Clin Sports Med 41:627–651
Pauyo T, Park JP, Bozzo I, Bernstein M (2022) Patellofemoral instability part I: evaluation and nonsurgical treatment. J Am Acad Orthop Surg 30:e1431–e1442
Qiu RY, Fitzpatrick DWD, Cohen D, Kay J, Almasri M, de Sa DL (2022) MRI as the optimal imaging modality for assessment and management of osteochondral fractures and loose bodies following traumatic patellar dislocation: a systematic review. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-07043-x
Rueth MJ, Koehl P, Schuh A, Goyal T, Wagner D (2022) Return to sports and short-term follow-up of 101 cases of medial patellofemoral ligament reconstruction using gracilis tendon autograft in children and adolescents. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-022-04365-w
Rund JM, Hinckel BB, Sherman SL (2021) Acute patellofemoral dislocation: controversial decision-making. Curr Rev Musculoskelet Med 14:82–87
Saccomanno MF, Maggini E, Vaisitti N, Pianelli A, Grava G, Cattaneo S, Milano G (2022) Sulcus angle, trochlear depth and Dejour’s classification can be reliably applied to evaluate trochlear dysplasia: a systematic review of radiological measurements. Arthroscopy. https://doi.org/10.1016/j.arthro.2022.08.039
Sillanpää PJ, Mäenpää HM (2012) First-time patellar dislocation: surgery or conservative treatment? Sports Med Arthrosc Rev 20:128–135
Smith TO, Chester R, Clark A, Donell ST, Stephenson R (2011) A national survey of the physiotherapy management of patients following first-time patellar dislocation. Physiotherapy 97:327–338
Tian G, Yang G, Zuo L, Li F, Wang F (2020) Conservative versus repair of medial patellofemoral ligament for the treatment of patients with acute primary patellar dislocations: a systematic review and meta-analysis. J Orthop Surg (Hong Kong) 28:2309499020932375
Watson R, Sullivan B, Stone AV, Jacobs C, Malone T, Heebner N, Noehren B (2022) Lateral patellar dislocation: a critical review and update of evidence-based rehabilitation practice guidelines and expected outcomes. JBJS Rev. https://doi.org/10.2106/JBJS.RVW.21.00159
Wierer G, Krabb N, Kaiser P, Ortmaier R, Schützenberger S, Schlumberger M, Hiller B, Ingruber F, Smekal V, Attal R, Seitlinger G (2022) The patellar instability probability calculator: a multivariate-based model to predict the individual risk of recurrent lateral patellar dislocation. Am J Sports Med 50:471–477
Xu Z, Song Y, Deng R, Zhang Z, Wang H, Yu JK (2022) Pathological thresholds of segmental femoral torsion in patients with patellar dislocation: influence on patellofemoral malalignment. Orthop J Sports Med 10:23259671221125216
Zhao Z, Wang Y, Li J, Wang H, Bai X, Wang Q, Li Z (2021) Clinical outcomes and prognostic factors in patients with recurrent patellar lateral dislocation treated with isolated medial patellofemoral ligament reconstruction: a retrospective single-center analysis. Orthop J Sports Med 9:2325967121995803
Zheng L, Ding HY, Feng Y, Sun BS, Zhu LL, Zhang GY (2021) Gender-related differences in concomitant articular injuries after acute lateral patellar dislocation. Injury 52:1549–1555
Acknowledgements
Special thanks to ESSKA, which enabled the dissemination of the survey, and thanks to all colleagues who completed the questionnaire. This study was supported and funded by the Italian Ministry of Health–“Ricerca Corrente”.
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent to participate
Participation to the study was voluntary and with no remuneration. No e-mail addresses or other identifying data were collected from all participants.
Consent to publish
All authors consent to the publication of the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
D’Ambrosi, R., Migliorini, F., Cerciello, S. et al. Management of the first episode of traumatic patellar dislocation: an international survey. Knee Surg Sports Traumatol Arthrosc 31, 2257–2265 (2023). https://doi.org/10.1007/s00167-022-07273-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-07273-z