Abstract
Purpose
Unexpected-positive-intraoperative-cultures (UPIC) are common in presumed aseptic revision-total-knee-arthroplasties (rTKA). However, the clinical significance is not entirely clear. In contrast, in some presumably septic rTKA, identification of an underlying pathogen was not possible, so-called unexpected-negative-intraoperative-cultures (UNIC). The purpose of this study was to evaluate the potential use of synovial alpha-defensin (AD) levels in these patients.
Methods
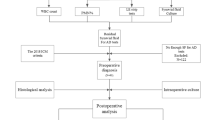
Synovial AD levels from 143 rTKAs were evaluated retrospectively from our prospectively maintained institutional periprostetic joint infection (PJI) biobank and database. The 2018-International Consensus Meeting (ICM) criteria was used to define the study groups. Samples from UPICs with a minimum of one positive intraoperative culture (ICM 2- ≥ 6) (n = 20) and UNIC’s (ICM ≥ 6) (n = 14) were compared to 34 septic culture-positive samples (ICM ≥ 6) and 75 aseptic culture-negative (ICM 0-1). Moreover, AD-lateral-flow-assay (ADLF) and an enzyme-linked-immunosorbent-assay (ELISA) in detecting the presence of AD in native and centrifuged synovial fluid specimens was performed. Concentration of AD determined by ELISA and ADLF methods, as well as microbiological, and histopathological results, serum and synovial parameters along with demographic factors were analysed.
Results
AD was positive in 31/34 (91.2%) samples from the septic culture-positive group and in 14/14 (100%) samples in the UNIC group. All UPIC samples showed a negative AD result. Positive AD samples were highly associated with culture positive and histopathological results (p < 0.001). No high-virulent microorganisms (0/20) were present in the UPIC group, compared to infected-group (19/34; 55.9%). High virulent microorganisms showed a positive AD result in 89.5% (17/19) of the cases. Methicillin resistant Staphylococcus epidermis (MRSE) infections had significantly higher AD levels than with methicillin susceptible S. epidermdis (MSSE) (p = 0.003). ELISA and ADLF tests were positive with centrifuged (8/8) and native (8/8) synovial fluid.
Conclusion
AD showed a solid diagnostic performance in infected and non-infected revisions, and it provided an additional value in the diagnosis of UPIC and UNIC associated to rTKAs. Pathogen virulence as well as antibiotic resistance pattern may have an effect on AD levels. Centrifugation of synovial fluid had no influence on ADLF results.


Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AD:
-
Alpha defensin
- ADLF:
-
Alpha-defensin-lateral-flow-assay
- BMI:
-
Body mass index
- CoNS:
-
Coagulase-negative Staphylococci
- CRP:
-
C-reactive protein
- DAIR:
-
Debridement-antibiotics and implant retention
- ELISA:
-
Enzyme-linked immunosorbent assay
- EUCAST:
-
European Committee on Antimicrobial Susceptibility Testing
- ICM:
-
2018-International Consensus Meeting
- M:
-
Mean
- Md:
-
Median
- MRSA:
-
Methicillin-resistant Staphylococcus aureus
- MRSE:
-
Methicillin-resistant Staphylococcus epidermidis
- MSSA:
-
Methicillin-susceptible Staphylococcus aureus
- MSSE:
-
Methicillin-susceptible Staphylococcus epidermidis
- PJI:
-
Periprosthetic joint infection
- PMN:
-
Polymorphonuclear percentage
- rTKA:
-
Revision total knee arthroplasty
- SD:
-
Standard deviation
- SLIM:
-
Synovial-like interface membrane
- TKA:
-
Total knee arthroplasty
- UNIC:
-
Unexpected negative intraoperative cultures
- UPIC:
-
Unexpected positive intraoperative cultures
- *:
-
p < 0.05
- **:
-
p < 0.001
References
Ahmad SS, Shaker A, Saffarini M, Chen AF, Hirschmann MT, Kohl S (2016) Accuracy of diagnostic tests for prosthetic joint infection: a systematic review. Knee Surgery Sport Traumatol Arthrosc 24:3064–3074
Bauer TW, Parvizi J, Kobayashi N, Krebs V (2006) Diagnosis of periprosthetic infection. J Bone Jt Surg 88:869–882
Bejon P, Berendt A, Atkins BL, Green N, Parry H, Masters S, Mclardy-Smith P, Gundle R, Byren I (2010) Two-stage revision for prosthetic joint infection: predictors of outcome and the role of reimplantation microbiology. J Antimicrob Chemother 65:569–575
Bonanzinga T, Zahar A, Dütsch M, Lausmann C, Kendoff D, Gehrke T (2017) How reliable is the alpha-defensin immunoassay test for diagnosing periprosthetic joint infection? A prospective study. Clin Orthop Relat Res 475:408–415
Deirmengian C, Kardos K, Kilmartin P, Gulati S, Citrano P, Booth RE (2015) The alpha-defensin test for periprosthetic joint infection responds to a wide spectrum of organisms. Clin Orthop Relat Res 473:2229–2235
Deirmengian C, Madigan J, Kallur Mallikarjuna S, Conway J, Higuera C, Patel R (2021) Validation of the alpha defensin lateral flow test for periprosthetic joint infection. J Bone Jt Surg 103:115–122
Drago L, Clerici P, Morelli I, Ashok J, Benzakour T, Bozhkova S, Alizadeh C, del Sel H, Sharma HK, Peel T, Mattina R, Romanò CL (2019) The World Association against Infection in Orthopaedics and Trauma (WAIOT) procedures for microbiological sampling and Processing for Periprosthetic Joint Infections (PJIs) and other implant-related infections. J Clin Med 8:933
European Committee on Antimicrobial Susceptibility Testing (2021) Breakpoint tables for interpretation of MICs and zone diameters Version 11.0.
Gatti G, Taddei F, Brandolini M, Mancini A, Denicolò A, Congestrì F, Manera M, Arfilli V, Battisti A, Zannoli S, Marino MM, Marzucco A, Morotti M, Grumiro L, Scalcione A, Dirani G, Cricca M, Sambri V (2022) Molecular approach for the laboratory diagnosis of periprosthetic joint infections. Microorganisms 10:1573
Hipfl C, Mooij W, Perka C, Hardt S, Wassilew GI (2021) Unexpected low-grade infections in revision hip arthroplasty for aseptic loosening. Bone Joint J 103-B:1070–1077
Hischebeth G, Randau T, Ploeger M, Friedrich M, Kaup E, Jacobs C, Molitor E, Hoerauf A, Gravius S, Wimmer M (2019) Staphylococcus aureus versus Staphylococcus epidermidis in periprosthetic joint infection—outcome analysis of methicillin-resistant versus methicillin-susceptible strains. Diagn Microbiol Infect Dis 93:125–130
Huard M, Detrembleur C, Poilvache H, Gyeels IP, Van Cauter M, Driesen R, Yombi J-C, Neyt J, Cornu O (2020) Alpha defensin: a diagnostic accuracy depending on the infection definition used. J Arthroplasty 35:1355–1360
Jacobs AME, Bénard M, Meis JF, van Hellemondt G, Goosen JHM (2017) The unsuspected prosthetic joint infection. Bone Joint J 99-B:1482–1489
Kalbian I, Park JW, Goswami K, Lee Y-K, Parvizi J, Koo K-H (2020) Culture-negative periprosthetic joint infection: prevalence, aetiology, evaluation, recommendations, and treatment. Int Orthop 44:1255–1261
Kleeman-Forsthuber LT, Dennis DA, Brady AC, Pollet AK, Johnson RM, Jennings JM (2021) Alpha-defensin is not superior to traditional diagnostic methods for detection of periprosthetic joint infection in total hip arthroplasty and total knee arthroplasty patients. J Arthroplasty 36:2144–2149
Kloos J, Vander Linden K, Vermote S, Berger P, Vandenneucker H (2022) Prevalence, interpretation, and management of unexpected positive cultures in revision TKA: a systematic review. Knee Surg Sport Traumatol Arthrosc 30(12):3998–4009. https://doi.org/10.1007/s00167-021-06856-6
Krenn V, Morawietz L, Perino G, Kienapfel H, Ascherl R, Hassenpflug GJ, Thomsen M, Thomas P, Huber M, Kendoff D, Baumhoer D, Krukemeyer MG, Natu S, Boettner F, Zustin J, Kölbel B, Rüther W, Kretzer JP, Tiemann A, Trampuz A, Frommelt L, Tichilow R, Söder S, Müller S, Parvizi J, Illgner U, Gehrke T (2014) Revised histopathological consensus classification of joint implant related pathology. Pathol Res Pract 210:779–786
Kuiper JWP, Verberne SJ, Vos SJ, van Egmond PW (2020) Does the alpha defensin ELISA test perform better than the alpha defensin lateral flow test for PJI Diagnosis? A systematic review and meta-analysis of prospective studies. Clin Orthop Relat Res 478:1333–1344
Lee YS, Koo K-H, Kim HJ, Tian S, Kim T-Y, Maltenfort MG, Chen AF (2017) Synovial fluid biomarkers for the diagnosis of periprosthetic joint infection. J Bone Jt Surg 99:2077–2084
Marson BA, Deshmukh SR, Grindlay DJC, Scammell BE (2018) Alpha-defensin and the synovasure lateral flow device for the diagnosis of prosthetic joint infection. Bone Joint J 100-B:703–711
McNally M, Sousa R, Wouthuyzen-Bakker M, Chen AF, Soriano A, Vogely HC, Clauss M, Higuera CA, Trebše R (2021) The EBJIS definition of periprosthetic joint infection. Bone Joint J 103-B:18–25
Milandt NR, Gundtoft PH, Overgaard S (2019) A single positive tissue culture increases the risk of rerevision of clinically aseptic THA: a national register study. Clin Orthop Relat Res 477:1372–1381
Neufeld ME, Lanting BA, Shehata M, Howard JL, MacDonald SJ, Teeter MG, Vasarhelyi EM (2021) Prevalence and outcomes of unexpected positive intraoperative cultures in presumed aseptic revision hip arthroplasty. J Bone Jt Surg Publ Ah 103:1392–1401
Parvizi J, Tan TL, Goswami K, Higuera C, Della Valle C, Chen AF, Shohat N (2018) The 2018 definition of periprosthetic hip and knee infection: an evidence-based and validated criteria. J Arthroplasty Churchill Livingstone Inc. 33:1309-1314 e2
Parvizi J, Tan TL, Goswami K, Higuera C, Della Valle C, Chen AF, Shohat N (2018) The 2018 definition of periprosthetic hip and knee infection: an evidence-based and validated criteria. J Arthroplasty 33:1309-1314.e2
Purudappa PP, Sharma OP, Priyavadana S, Sambandam S, Villafuerte JA (2020) Unexpected positive intraoperative cultures (UPIC) in revision Hip and knee arthroplasty- a review of the literature. J Orthop 17:1–6
Sigmund IK, Holinka J, Lang S, Stenicka S, Staats K, Hobusch G, Kubista B, Windhager R (2019) A comparative study of intraoperative frozen section and alpha defensin lateral flow test in the diagnosis of periprosthetic joint infection. Acta Orthop 90:105–110
van Sloten M, Gómez-Junyent J, Ferry T, Rossi N, Petersdorf S, Lange J, Corona P, Araújo Abreu M, Borens O, Zlatian O, Soundarrajan D, Rajasekaran S, Wouthuyzen-Bakker M (2022) Should all patients with a culture-negative periprosthetic joint infection be treated with antibiotics? Bone Joint J 104-B:183–188
Tan TL, Kheir MM, Shohat N, Tan DD, Kheir M, Chen C, Parvizi J (2018) Culture-negative periprosthetic joint infection. JBJS Open Access 3:e0060
Author information
Authors and Affiliations
Contributions
All authors had full access to the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Have made substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data: SS, BJHF, AA, MD, MK, JAM, SGH; JGH. Have been involved in drafting the manuscript or revising it critically for important intellectual content SS, BJHF, AA, MD, MK, JAM, SGH, JGH. Have given final approval of the version to be published SS, BJHF, AA, MD, MK, JAM, SGH, JGH. Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. SS, BJHF, AA, MD, MK, JAM, SGH, JGH.
Corresponding author
Ethics declarations
Conflict of interest
The institution of one or more of the authors (S.S., B.J.H.F., A.A., M.D., M.K., J.A.M., S.G.H; J.G.H.) has received funding from Zimmer Biomet. Zimmer Biomet covered the costs of Synovasure® Alpha Defensin Lateral Flow and Synovasure® Alpha Defensin ELISA Laboratory Test.
Ethical approval
A retrospective analysis from synovial fluid samples of revision and re-revision TKAs of our prospectively collected biobank (2016–2021) was performed.
Funding
The authors certify that they do not have affiliations with or involvement in any organization or entity with any financial or non-financial interest in the subject or materials discussed in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Simon, S., Frank, B.J.H., Aichmair, A. et al. Alpha-defensin as a diagnostic tool in revision total knee arthroplasties with unexpected positive intraoperative cultures and unexpected culture negative intraoperative cultures. Knee Surg Sports Traumatol Arthrosc 31, 1462–1469 (2023). https://doi.org/10.1007/s00167-022-07268-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-07268-w