Abstract
Purpose
The purpose of this study was to evaluate the effects of arthroscopic meniscal centralization reinforcement for a medial meniscus (MM) posterior root defect on knee kinematics and meniscal extrusion in the anterior cruciate ligament reconstructed (ACLR) knee.
The hypothesis was that the medial meniscus centralization would reduce extrusion and anterior laxity in ACLR knee with a medical meniscal defect.
Methods
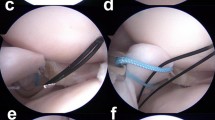
Fourteen fresh-frozen human cadaveric knees were tested using a six-degrees-of-freedom robotic system under the following loading conditions: (a) an 89.0 N anterior tibial load, (b) 5.0 Nm internal and external rotational torques, (c) a 10.0 Nm valgus and varus loadings, and (d) a combined 7.0 Nm valgus moment and then a 5.0 Nm internal rotation torque as a static simulated pivot shift. The tested knee states included: (1) anatomic single-bundle cruciate ligament reconstruction with intact medial meniscus (MM Intact), (2) anatomic single-bundle cruciate ligament reconstruction with medial meniscus posterior root defect (MM Defect), (3) Anatomic single-bundle cruciate ligament reconstruction with medial meniscus arthroscopic centralization (MM Centralization). Medial meniscus arthroscopic centralization was performed using 1.4 mm anchors with #2 suture. The MM extrusion (MME) was measured using ultrasound under unloaded and varus loading conditions at 0° and 30° of flexion.
Results
Anterior tibial translation (ATT) increased significantly with MM posterior root defect compared to MM intact at all flexion angles. With MM centralization, ATT was not significantly different from the intact meniscus at 15° and 30° of flexion. Meniscus extrusion increased significantly with the root defect compared to intact meniscus and decreased significantly with meniscal centralization compared to the root defect at both flexion angles.
Conclusions
In ACL reconstruction, cases involving irreparable medial meniscal posterior root tears, applying arthroscopic centralization for avoiding the meniscal extrusion should be considered. Clinically, in ACL reconstruction cases with irreparable medial meniscal posterior root tears, applying arthroscopic meniscal centralization for avoiding the meniscal extrusion should be considered. Meniscal centralization decreases the extrusion of the MM and offers improvements in knee laxity.







Similar content being viewed by others
References
Allaire R, Muriuki M, Gilbertson L, Harner CD (2008) Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am 90:1922–1931
Araujo PH, Asai S, Pinto M, Protta T, Middleton K, Linde-Rosen M et al (2015) ACL graft position affects in situ graft force following ACL reconstruction. J Bone Joint Surg Am 97:1767–1773
Brody JM, Lin HM, Hulstyn MJ, Tung GA (2006) Lateral meniscus root tear and meniscus extrusion with anterior cruciate ligament tear. Radiology 239:805–810
Daney BT, Aman ZS, Krob JJ, Storaci HW, Brady AW, Nakama G et al (2019) Utilization of transtibial centralization suture best minimizes extrusion and restores tibiofemoral contact mechanics for anatomic medial meniscal root repairs in a cadaveric model. Am J Sports Med 47:1591–1600
Debieux P, Jimenez AE, Novaretti JV, Kaleka CC, Kriscenski DE, Astur DC et al (2021) Medial meniscal extrusion greater than 4 mm reduces medial tibiofemoral compartment contact area: a biomechanical analysis of tibiofemoral contact area and pressures with varying amounts of meniscal extrusion. Knee Surg Sports Traumatol Arthrosc 29:3124–3132
DePhillipo NN, Moatshe G, Brady A, Chahla J, Aman ZS, Dornan GJ et al (2018) Effect of meniscocapsular and meniscotibial lesions in ACL-deficient and ACL-reconstructed knees: a biomechanical study. Am J Sports Med 46:2422–2431
Faul F, Erdfelder E, Lang AG, Buchner A (2007) G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39:175–191
Gale DR, Chaisson CE, Totterman SM, Schwartz RK, Gale ME, Felson D (1999) Meniscal subluxation: association with osteoarthritis and joint space narrowing. Osteoarthritis Cartilage 7:526–532
Jenkins ND, Miller JM, Buckner SL, Cochrane KC, Bergstrom HC, Hill EC et al (2015) Test-retest reliability of single transverse versus panoramic ultrasound imaging for muscle size and echo intensity of the biceps brachii. Ultrasound Med Biol 41:1584–1591
Jones AO, Houang MT, Low RS, Wood DG (2006) Medial meniscus posterior root attachment injury and degeneration: MRI findings. Australas Radiol 50:306–313
Kanamori A, Zeminski J, Rudy TW, Li G, Fu FH, Woo SL (2002) The effect of axial tibial torque on the function of the anterior cruciate ligament: a biomechanical study of a simulated pivot shift test. Arthroscopy 18:394–398
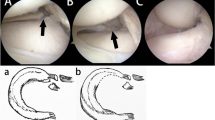
Koga H, Muneta T, Yagishita K, Watanabe T, Mochizuki T, Horie M et al (2012) Arthroscopic centralization of an extruded lateral meniscus. Arthrosc Tech 1:e209-212
Koga H, Watanabe T, Horie M, Katagiri H, Otabe K, Ohara T et al (2017) Augmentation of the pullout repair of a medial meniscus posterior root tear by arthroscopic centralization. Arthrosc Tech 6:e1335–e1339
Kohno Y, Koga H, Ozeki N, Matsuda J, Mizuno M, Katano H et al (2022) Biomechanical analysis of a centralization procedure for extruded lateral meniscus after meniscectomy in porcine knee joints. J Orthop Res 40:1097–1103
Kondo E, Merican AM, Yasuda K, Amis AA (2010) Biomechanical comparisons of knee stability after anterior cruciate ligament reconstruction between 2 clinically available transtibial procedures: anatomic double bundle versus single bundle. Am J Sports Med 38:1349–1358
Kopf S, Beaufils P, Hirschmann MT, Rotigliano N, Ollivier M, Pereira H et al (2020) Management of traumatic meniscus tears: the 2019 ESSKA meniscus consensus. Knee Surg Sports Traumatol Arthrosc 28:1177–1194
Kubota R, Koga H, Ozeki N, Matsuda J, Kohno Y, Mizuno M et al (2020) The effect of a centralization procedure for extruded lateral meniscus on load distribution in porcine knee joints at different flexion angles. BMC Musculoskelet Disord 21:1–8
Leafblad ND, Smith PA, Stuart MJ, Krych AJ (2021) Arthroscopic centralization of the extruded medial meniscus. Arthrosc Tech 10:e43–e48
Lerer DB, Umans HR, Hu MX, Jones MH (2004) The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol 33:569–574
Liu Y, Joseph GB, Foreman SC, Li X, Lane NE, Nevitt MC et al (2021) Determining a threshold of medial meniscal extrusion for prediction of knee pain and cartilage damage progression over 4 years: data from the osteoarthritis initiative. AJR Am J Roentgenol 216:1318–1328
Makiev KG, Vasios IS, Georgoulas P, Tilkeridis K, Drosos G, Ververidis A (2022) Clinical significance and management of meniscal extrusion in different knee pathologies: a comprehensive review of the literature and treatment algorithm. Knee Surg Relat Res 34:1–11
Matheny LM, Ockuly AC, Steadman JR, LaPrade RF (2015) Posterior meniscus root tears: associated pathologies to assist as diagnostic tools. Knee Surg Sports Traumatol Arthrosc 23:3127–3131
Mochizuki Y, Kawahara K, Samejima Y, Kaneko T, Ikegami H, Musha Y (2021) Short-term results and surgical technique of arthroscopic centralization as an augmentation for medial meniscus extrusion caused by medial meniscus posterior root tear. Eur J Orthop Surg Traumatol 31:1235–1241
Nakamura R, Takahashi M, Kuroda K, Katsuki Y (2018) Suture anchor repair for a medial meniscus posterior root tear combined with arthroscopic meniscal centralization and open wedge high tibial osteotomy. Arthrosc Tech 7:e755–e761
Nakamura T, Marshall BD, Price TM, Mao Y, Linde MA, Koga H et al (2021) Arthroscopic centralization for lateral meniscal injuries reduces laxity in the anterior cruciate ligament-reconstructed knee. Am J Sports Med 49:3528–3533
Ozeki N, Muneta T, Kawabata K, Koga H, Nakagawa Y, Saito R et al (2017) Centralization of extruded medial meniscus delays cartilage degeneration in rats. J Orthop Sci 22:542–548
Ozeki N, Seil R, Krych AJ, Koga H (2021) Surgical treatment of complex meniscus tear and disease: state of the art. J ISAKOS 6:35–45
Sasaki Y, Fujii M, Araki D, Marshall BD, Linde MA, Smolinski P et al (2021) Effect of percentage of femoral anterior cruciate ligament insertion site reconstructed with hamstring tendon on knee kinematics and graft force. Am J Sports Med 49:1279–1285
Vedi V, Williams A, Tennant SJ, Spouse E, Hunt DM, Gedroyc WM (1999) Meniscal movement. An in-vivo study using dynamic MRI. J Bone Joint Surg Br 81:37–41
Widmer S, Steiner RP, Morscher MA, Shasti M, Weiner DS, Adamczyk MJ et al (2019) An investigation to validate the equivalence of physes obtained from different anatomic regions in a single animal species: Implications for choosing experimental controls in clinical studies. Bone Rep 10:100209
Xu Y, Liu J, Kramer S, Martins C, Kato Y, Linde-Rosen M et al (2011) Comparison of in situ forces and knee kinematics in anteromedial and high anteromedial bundle augmentation for partially ruptured anterior cruciate ligament. Am J Sports Med 39:272–278
Acknowledgements
In memoriam and appreciation of Dr. Freddie H. Fu (1950-2021).
Funding
Department of Orthopedic Surgery.
Author information
Authors and Affiliations
Contributions
HU, RK, ML, MD, and PS: were involved in the study design and data interpretation. HU, RK, ML, MD, and PS: were involved in the data analysis. HU, RK, ML, MD, and PS: critically revised the report, commented on drafts of the manuscript, and approved the final report. HU, RK, ML, MD, and PS: revised the manuscript, approved the manuscript to be published, and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Ethical approval
Institutional approval (Committee for Oversight of Research and Clinical training Involving Decedents #1055).
Informed consent
NA.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ueki, H., Kanto, R., DiNenna, M. et al. Arthroscopic centralization reduces extrusion of the medial meniscus with posterior root defect in the ACL reconstructed knee. Knee Surg Sports Traumatol Arthrosc 31, 543–550 (2023). https://doi.org/10.1007/s00167-022-07160-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-07160-7