Abstract
Purpose
Medial meniscus posterior root tears (MMPRTs) occur most frequently in middle-aged and older adults. However, this serious condition can also occur in younger patients. The purpose of this study was to compare anterior cruciate ligament (ACL) degeneration and sagittal medial tibial slope in young adults with and without MMPRT.
Methods
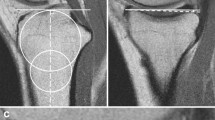
Eighteen healthy volunteers, 18 young patients (20–49 years of age), and 30 middle-aged and older patients (50–70 years of age) with MMPRT repair were included in the study. Sex, body mass index (BMI), femorotibial angle, ACL degeneration, and medial tibial slope angle were compared among the groups. ACL degeneration and medial tibial slope angle were assessed using magnetic resonance imaging.
Results
In the healthy volunteer group, the young patient group, and the older patient group, the medial tibial slopes were 3.5° ± 1.4°, 6.1° ± 2.7°, and 7.2° ± 1.9°, respectively, and the ACL degeneration rates were 5.6%, 38.9%, and 43.3%, respectively. Young patients with MMPRT had significantly steeper medial tibial slopes and ACL degeneration compared to those of the healthy volunteers (P < 0.05). The parameters of young patients were similar to those of older patients with MMPRT. In the multivariate logistic regression analysis, BMI, medial tibial slope, and ACL degeneration were significantly associated with MMPRT in young patients.
Conclusion
BMI, steep medial tibial slope, and ACL degeneration contribute to MMPRT development in younger patients.
Level of evidence
Level III.



Similar content being viewed by others
Code availability
Not applicable.
References
Bae JH, Paik NH, Park GW, Yoon JR, Chae DJ, Kwon JH et al (2013) Predictive value of painful popping for a posterior root tear of the medial meniscus in middle-aged to older Asian patients. Arthroscopy 29:545–549
Bhatia S, LaPrade CM, Ellman MB, LaPrade RF (2014) Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med 42:3016–3030
Bin SI, Kim JM, Shin SJ (2004) Radial tears of the posterior horn of the medial meniscus. Arthroscopy 20:373–378
Boyd KT, Myers PT (2003) Meniscus preservation; rationale, repair techniques and results. Knee 10:1–11
Celikyay F, Yuksekkaya R, Bilgic E (2020) A retrospective comparison of ACL tear and mucoid degeneration MRI findings and an emphasis on evaluating of ACL, Blumensaat, and PCL angles. J Belgian Soc Radiol 104:1–8
Chung KS, Ha JK, Ra HJ, Kim JG (2016) Prognostic factors in the midterm results of pullout fixation for posterior root tears of the medial meniscus. Arthroscopy 32:1319–1327
Chahla J, LaPrade RF (2019) Meniscal root tears. Arthroscopy 35:1304–1305
Choi SH, Bae S, Ji SK, Chang MJ (2012) The MRI findings of meniscal root tear of the medial meniscus: emphasis on coronal, sagittal and axial images. Knee Surg Sports Traumatol Arthrosc 20:2098–2103
Choi JY, Chang EY, Cunha GM, Tafur M, Statum S, Chung CB (2014) Posterior medial meniscus root ligament lesions: MRI classification and associated findings. AJR Am J Roentgenol 203:1286–1292
Furumatsu T, Fujii M, Kodama Y, Ozaki T (2017) A giraffe neck sign of the medial meniscus: a characteristic finding of the medial meniscus posterior root tear on magnetic resonance imaging. J Orthop Sci 22:731–736
Furumatsu T, Okazaki Y, Okazaki Y, Hino T, Kamatsuki Y, Masuda S et al (2019) Injury patterns of medial meniscus posterior root tears. Orthop Traumatol Surg Res 105:107–111
Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD (2004) Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med 32:376–382
Hiranaka T, Furumatsu T, Okazaki Y, Yamawaki T, Okazaki Y, Kodama Y et al (2021) Steep medial tibial slope and prolonged delay to surgery are associated with bilateral medial meniscus posterior root tear. Knee Surg Sports Traumatol Arthrosc 29:1052–1057
Hwang BY, Kim SJ, Lee SW, Lee HE, Lee CK, Hunter DJ et al (2012) Risk factors for medial meniscus posterior root tear. Am J Sports Med 40:1606–1610
Imhoff FB, Mehl J, Comer BJ, Obopilwe E, Cote MP, Feucht MJ et al (2019) Slope-reducing tibial osteotomy decrease ACL-graft forces and anterior tibial translation under axial load. Knee Surg Sports Traumatol Arthrosc 27:3381–3389
Inoue H, Furumatsu T, Miyazawa S, Fujii M, Kodama Y, Ozaki T (2018) Improvement in the medial meniscus posterior shift following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 26:434–441
Kodama Y, Furumatsu T, Okazaki Y, Takihira S, Hiranaka T, Miyazawa S et al (2021) Transtibial pullout repair of medial meniscus posterior root tears: effects on the meniscus healing score and ICRS grade among patients with mild osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc 29:3001–3009
Lin LJ, Akpinar B, Meislin RJ (2020) Tibial slope and anterior cruciate ligament reconstruction outcomes. JBJS Rev 8(4):e0184
Lee JI, Kim DH, Choi HG, Kim TW, Lee YS (2021) Analysis of affecting factors of the fate of medial meniscus posterior root tear based on treatment strategies. J Clin Med 10:1–12
Marouane H, Shirazi-Adl A, Hashemi J (2015) Quantification of the role of tibial posterior slope in knee joint mechanics and ACL force in simulated gait. J Biomech 48:1899–1905
Masuda S, Furumatsu T, Okazaki Y, Kodama Y, Hino T, Kamatsuki Y et al (2018) Medial meniscus posterior root tear induces pathological posterior extrusion of the meniscus in the knee-flexed position: an open magnetic resonance imaging analysis. Orthop Traumatol Surg Res 104:485–489
McIntyre J, Moelleken S, Tirman P (2001) Mucoid degeneration of the anterior cruciate ligament mistaken for ligamentous tears. Skeletal Radiol 30:312–315
Meier M, Janssen D, Koeck FX, Thienpont E, Beckmann J, Best R (2021) Variations in medial and lateral slope and medial proximal tibial angle. Knee Surg Sports Traumatol Arthrosc 29:939–946
Okazaki Y, Furumatsu T, Kodama Y, Kamatsuki Y, Okazaki Y, Hiranaka T et al (2021) Steep posterior slope and shallow concave shape of the medial tibial plateau are risk factors for medial meniscus posterior root tears. Knee Surg Sports Traumatol Arthrosc 29:44–50
Okazaki Y, Furumatsu T, Miyazawa S, Kodama Y, Kamatsuki Y, Hino T et al (2019) Meniscal repair concurrent with anterior cruciate ligament reconstruction restores posterior shift of the medial meniscus in the knee-flexed position. Knee Surg Sports Traumatol Arthrosc 27:361–368
Ogawa H, Matsumoto K, Akiyama H (2021) Functional assessment of the anterior cruciate ligament in knee osteoarthritis. J Orthop 23:175–179
Ozkoc G, Circi E, Gonc U, Irgit K, Pourbagher A, Tandogan RN (2008) Radial tears in the root of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc 16:849–854
Papadopoulou P (2007) The celery stalk sign. Radiology 245:916–917
Papageorgiou CD, Gil JE, Kanamori A, Fenwick JA, Woo SL, Fu FH (2001) The biomechanical interdependence between the anterior cruciate ligament replacement graft and the medial meniscus. Am J Sports Med 29:226–231
Kwee RM, Hafezi-Nejad N, Roemer FW, Zikria BA, Hunter DJ, Guermazi A et al (2018) Association of mucoid degeneration of the anterior cruciate ligament at MR imaging with medial tibiofemoral osteoarthritis progression at radiography: data from the osteoarthritis initiative. Radiology 287:912–921
Samuelsen BT, Aman ZS, Kennedy MI, Dornan GJ, Storaci HW, Brady AW et al (2020) Posterior medial meniscus root tears potentiate the effect of increased tibial slope on anterior cruciate ligament graft forces. Am J Sports Med 48:334–340
Shelburne KB, Kim HJ, Sterett WI, Pandy MG (2011) Effect of posterior tibial slope on knee biomechanics during functional activity. J Orthop Res 29:223–231
Sung K, Jeong C, Ha K, Jong H, Han R, Lee S et al (2018) Pullout fixation for medial meniscus posterior root tears : clinical results were not age-dependent, but osteoarthritis progressed. Knee Surg Sport Traumatol Arthrosc 27:189–196
Zhang X, Furumatsu T, Okazaki Y, Hiranaka T, Kodama Y, Xue H et al (2021) High body mass index is a risk factor for unfavorable clinical outcomes after medial meniscus posterior root repair in well-aligned knees. J Orthop Sci 26:430–434
Acknowledgements
We would like to thank Editage (www.editage.jp) for English language editing.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
TF: designed the study. MT, YO, and TH: contributed to the analysis and interpretation of data. All authors have contributed to data collection and interpretation and critically reviewed the manuscript. All authors approved the final version of the manuscript and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review board.
Consent to participate
Informed consent was obtained from all individual participants included in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kodama, Y., Furumatsu, T., Tamura, M. et al. Steep posterior slope of the medial tibial plateau and anterior cruciate ligament degeneration contribute to medial meniscus posterior root tears in young patients. Knee Surg Sports Traumatol Arthrosc 31, 279–285 (2023). https://doi.org/10.1007/s00167-022-07095-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-07095-z