Abstract
Purpose
Objectives are (1) to evaluate the biomechanical effect of isolated medial patellofemoral ligament (MPFL) reconstruction in the setting of increased tibial tuberosity–trochlear groove distance (TTTG), in terms of patella contact pressures, contact area and lateral displacement; (2) to describe the threshold of TTTG up to which MPFL reconstruction should be performed alone or in combination with tibial tuberosity transfer.
Methods
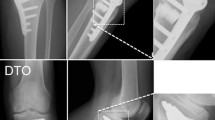
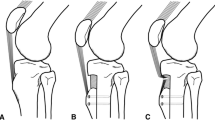
A finite element model of the knee was developed and validated. The model was modified to simulate isolated MPFL reconstruction, tibial tuberosity transfer and MPFL reconstruction combined with tibial tuberosity transfer for patella malalignment. Two TT–TG distances (17 mm and 22 mm) were simulated. Patella contact pressure, contact area and lateral displacement were analysed.
Results
Isolated MPFL reconstruction, at early degrees of flexion, restored normal patella contact pressure when TTTG was 17 mm, but not when TTTG was 22 mm. After 60° of flexion, the TTTG distance was the main factor influencing contact pressure. Isolated MPFL reconstruction for both TTTG 17 mm and 22 mm showed higher contact area and lower lateral displacement than normal throughout knee flexion. Tibial tuberosity transfer, at early degrees of flexion, reduced the contact pressure, but did not restore the normal contact pressure. After 60° of flexion, the TTTG distance was the main factor influencing contact pressure. Tibial tuberosity transfer maintained lower contact area than normal throughout knee flexion. The lateral displacement was higher than normal between 0° and 30° of flexion (< 0.5 mm). MPFL reconstruction combined with tibial tuberosity transfer produced the same contact mechanics and kinematics of the normal condition.
Conclusion
This study highlights the importance of considering to correct alignment in lateral tracking patella to avoid focal patella overload. Our results showed that isolated MPFL reconstruction corrects patella kinematics regardless of TTTG distance. However, isolated MPFL reconstruction would not restore normal patella contact pressure when TTTG is 22 mm. For TTTG 22 mm, the combined procedure of MPFL reconstruction and tibial tuberosity transfer provided an adequate patellofemoral contact mechanics and kinematics, restoring normal biomechanics. This data supports the use of MPFL reconstruction when the patient has normal alignment and the use of combined MPFL reconstruction and tibial tuberosity transfer in patients with elevated TT–TG distances to avoid focal overload.



Similar content being viewed by others
References
Alvarez O, Steensen RN, Rullkoetter PJ, Fitzpatrick CK (2020) Computational approach to correcting joint instability in patients with recurrent patellar dislocation. J Orthop Res 38:768–776
Anderson G, Diduch DR (2022) Medial patellofemoral ligament reconstruction: tips and tricks to get it right. Clin Sports Med 41:89–96
Balcarek P, Jung K, Frosch KH, Sturmer KM (2011) Value of the tibial tuberosity-trochlear groove distance in patellar instability in the young athlete. Am J Sports Med 39:1756–1761
Beck AP, Kliethermes SA, Trotter CA, Lang PJ, Scerpella TA (2022) Medial patellofemoral ligament repair for recurrent patellar instability: successful outcomes among patients with low coronal malalignment and normal patellar height. Orthopedics 45:e23–e29
Chahla J, Smigielski R, LaPrade RF, Fulkerson JP (2019) An updated overview of the anatomy and function of the proximal medial patellar restraints (medial patellofemoral ligament and the medial quadriceps tendon femoral ligament). Sports Med Arthrosc Rev 27:136–142
Churchill DL, Incavo SJ, Johnson CC, Beynnon BD (1998) The transepicondylar axis approximates the optimal flexion axis of the knee. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-199811000-00016111-118
Dall’Oca C, Elena N, Lunardelli E, Ulgelmo M, Magnan B (2020) MPFL reconstruction: indications and results. Acta Biomed 91:128–135
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2:19–26
Elias JJ, Cosgarea AJ (2006) Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage: a computational analysis. Am J Sports Med 34:1478–1485
Elias JJ, Jones KC, Copa AJ, Cosgarea AJ (2018) Computational simulation of medial versus anteromedial tibial tuberosity transfer for patellar instability. J Orthop Res 36:3231–3238
Elias JJ, Jones KC, Cyrus Rezvanifar S, Gabra JN, Morscher MA, Cosgarea AJ (2018) Dynamic tracking influenced by anatomy following medial patellofemoral ligament reconstruction: computational simulation. Knee 25:262–270
Elias JJ, Jones KC, Lalonde MK, Gabra JN, Rezvanifar SC, Cosgarea AJ (2018) Allowing one quadrant of patellar lateral translation during medial patellofemoral ligament reconstruction successfully limits maltracking without overconstraining the patella. Knee Surg Sports Traumatol Arthrosc 26:2883–2890
Farahmand F, Senavongse W, Amis AA (1998) Quantitative study of the quadriceps muscles and trochlear groove geometry related to instability of the patellofemoral joint. J Orthop Res 16:136–143
Farahmand F, Tahmasbi MN, Amis AA (1998) Lateral force-displacement behaviour of the human patella and its variation with knee flexion–a biomechanical study in vitro. J Biomech 31:1147–1152
Fulkerson JP (2018) Editorial commentary: medial patellofemoral ligament reconstruction alone works well when the patient has normal alignment, but don’t forget to move the tibial tubercle when necessary! Arthroscopy 34:1355–1357
Gardner EC, Molho DA, Fulkerson JP (2022) Coronal malalignment-when and how to perform a tibial tubercle osteotomy. Clin Sports Med 41:15–26
Haut Donahue TL, Hull ML, Rashid MM, Jacobs CR (2003) How the stiffness of meniscal attachments and meniscal material properties affect tibio-femoral contact pressure computed using a validated finite element model of the human knee joint. J Biomech 36:19–34
Herbort M, Hoser C, Domnick C, Raschke MJ, Lenschow S, Weimann A et al (2014) MPFL reconstruction using a quadriceps tendon graft: part 1: biomechanical properties of quadriceps tendon MPFL reconstruction in comparison to the Intact MPFL. A human cadaveric study. Knee 21:1169–1174
Homyk A, Orsi A, Wibby S, Yang N, Nayeb-Hashemi H, Canavan PK (2012) Failure locus of the anterior cruciate ligament: 3D finite element analysis. Comput Methods Biomech Biomed Engin 15:865–874
Hurley ET, Colasanti CA, Anil U, McAllister D, Matache BA, Alaia MJ et al (2021) Management of patellar instability: a network meta-analysis of randomized control trials. Am J Sports Med. https://doi.org/10.1177/036354652110200003635465211020000
Kay J, Memon M, Ayeni OR, Peterson D (2021) Medial patellofemoral ligament reconstruction techniques and outcomes: a scoping review. Curr Rev Musculoskelet Med 14:321–327
Kheir N, Salvatore G, Berton A, Orsi A, Egan J, Mohamadi A et al (2022) Lateral release associated with MPFL reconstruction in patients with acute patellar dislocation. BMC Musculoskelet Disord 23:139
Kiapour A, Kiapour AM, Kaul V, Quatman CE, Wordeman SC, Hewett TE et al (2014) Finite element model of the knee for investigation of injury mechanisms: development and validation. J Biomech Eng 136:011002
Kita K, Tanaka Y, Toritsuka Y, Amano H, Uchida R, Shiozaki Y et al (2017) 3D computed tomography evaluation of morphological changes in the femoral tunnel after medial patellofemoral ligament reconstruction with hamstring tendon graft for recurrent patellar dislocation. Am J Sports Med 45:1599–1607
Kusayama T, Harner CD, Carlin GJ, Xerogeanes JW, Smith BA (1994) Anatomical and biomechanical characteristics of human meniscofemoral ligaments. Knee Surg Sports Traumatol Arthrosc 2:234–237
Lenschow S, Schliemann B, Gestring J, Herbort M, Schulze M, Kosters C (2013) Medial patellofemoral ligament reconstruction: fixation strength of 5 different techniques for graft fixation at the patella. Arthroscopy 29:766–773
Liu Z, Yi Q, He L, Yao C, Zhang L, Lu F et al (2021) Comparing nonoperative treatment, MPFL repair, and MPFL reconstruction for patients with patellar dislocation: a systematic review and network meta-analysis. Orthop J Sports Med 9:23259671211026624
Longo UG, Berton A, Salvatore G, Migliorini F, Ciuffreda M, Nazarian A et al (2016) Medial patellofemoral ligament reconstruction combined with bony procedures for patellar instability: current indications, outcomes, and complications. Arthroscopy. https://doi.org/10.1016/j.arthro.2016.01.013
Longo UG, Ciuffreda M, Locher J, Berton A, Salvatore G, Denaro V (2017) Treatment of primary acute patellar dislocation: systematic review and quantitative synthesis of the literature. Clin J Sport Med 27:511–523
Longo UG, Rizzello G, Ciuffreda M, Loppini M, Baldari A, Maffulli N et al (2016) Elmslie-Trillat, Maquet, Fulkerson, Roux Goldthwait, and Other distal realignment procedures for the management of patellar dislocation: systematic review and quantitative synthesis of the literature. Arthroscopy 32:929–943
Longo UG, Vincenzo C, Mannering N, Ciuffreda M, Salvatore G, Berton A et al (2018) Trochleoplasty techniques provide good clinical results in patients with trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc 26:2640–2658
Merican AM, Amis AA (2009) Iliotibial band tension affects patellofemoral and tibiofemoral kinematics. J Biomech 42:1539–1546
Merican AM, Kondo E, Amis AA (2009) The effect on patellofemoral joint stability of selective cutting of lateral retinacular and capsular structures. J Biomech 42:291–296
Merican AM, Sanghavi S, Iranpour F, Amis AA (2009) The structural properties of the lateral retinaculum and capsular complex of the knee. J Biomech 42:2323–2329
Middleton KK, Gruber S, Shubin Stein BE (2019) Why and where to move the tibial tubercle: indications and techniques for tibial tubercle osteotomy. Sports Med Arthrosc Rev 27:154–160
Migliorini F, Eschweiler J, Betsch M, Knobe M, Tingart M, Maffulli N (2021) Prognostic factors for isolated medial patellofemoral ligament reconstruction: a systematic review. Surgeon. https://doi.org/10.1016/j.surge.2021.03.003
Migliorini F, Oliva F, Maffulli GD, Eschweiler J, Knobe M, Tingart M et al (2021) Isolated medial patellofemoral ligament reconstruction for recurrent patellofemoral instability: analysis of outcomes and risk factors. J Orthop Surg Res 16:239
Migliorini F, Trivellas A, Eschweiler J, Knobe M, Tingart M, Maffulli N (2022) Comparable outcome for autografts and allografts in primary medial patellofemoral ligament reconstruction for patellofemoral instability: systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 30:1282–1291
Mononen ME, Mikkola MT, Julkunen P, Ojala R, Nieminen MT, Jurvelin JS et al (2012) Effect of superficial collagen patterns and fibrillation of femoral articular cartilage on knee joint mechanics-a 3D finite element analysis. J Biomech 45:579–587
Mulliez A, Lambrecht D, Verbruggen D, Van Der Straeten C, Verdonk P, Victor J (2015) Clinical outcome in MPFL reconstruction with and without tuberositas transposition. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-015-3654-0
Nomura E (1999) Classification of lesions of the medial patello-femoral ligament in patellar dislocation. Int Orthop 23:260–263
Orsi AD, Canavan PK, Vaziri A, Goebel R, Kapasi OA, Nayeb-Hashemi H (2017) The effects of graft size and insertion site location during anterior cruciate ligament reconstruction on intercondylar notch impingement. Knee 24:525–535
Radcliffe IA, Prescott P, Man HS, Taylor M (2007) Determination of suitable sample sizes for multi-patient based finite element studies. Med Eng Phys 29(10):1065–1072
Redler LH, Meyers KN, Brady JM, Dennis ER, Nguyen JT, Shubin Stein BE (2018) Anisometry of Medial patellofemoral ligament reconstruction in the setting of increased tibial tubercle-trochlear groove distance and patella alta. Arthroscopy 34:502–510
Salvatore G, Berton A, Orsi A, Egan J, Walley KC, Johns WL et al (2022) Lateral release with tibial tuberosity transfer alters patellofemoral biomechanics promoting multidirectional patellar instability. Arthroscopy 38:953–964
Shah KS, Saranathan A, Koya B, Elias JJ (2015) Finite element analysis to characterize how varying patellar loading influences pressure applied to cartilage: model evaluation. Comput Methods Biomech Biomed Engin 18:1509–1515
Steensen RN, Bentley JC, Trinh TQ, Backes JR, Wiltfong RE (2015) The prevalence and combined prevalences of anatomic factors associated with recurrent patellar dislocation: a magnetic resonance imaging study. Am J Sports Med 43:921–927
Stephen JM, Dodds AL, Lumpaopong P, Kader D, Williams A, Amis AA (2015) The ability of medial patellofemoral ligament reconstruction to correct patellar kinematics and contact mechanics in the presence of a lateralized tibial tubercle. Am J Sports Med 43:2198–2207
Stephen JM, Kader D, Lumpaopong P, Deehan DJ, Amis AA (2013) Sectioning the medial patellofemoral ligament alters patellofemoral joint kinematics and contact mechanics. J Orthop Res 31:1423–1429
Stephen JM, Kaider D, Lumpaopong P, Deehan DJ, Amis AA (2014) The effect of femoral tunnel position and graft tension on patellar contact mechanics and kinematics after medial patellofemoral ligament reconstruction. Am J Sports Med 42:364–372
Su P, Hu H, Li S, Xu T, Li J, Fu W (2022) Tibial tubercle-trochlear groove/trochlear width is the optimal indicator for diagnosing a lateralized tibial tubercle in recurrent patellar dislocation requiring surgical stabilization. Arthroscopy 38:1288–1298
Tensho K, Akaoka Y, Shimodaira H, Takanashi S, Ikegami S, Kato H et al (2015) What components comprise the measurement of the tibial tuberosity-trochlear groove distance in a patellar dislocation population? J Bone Jt Surg Am 97:1441–1448
Yang NH, Canavan PK, Nayeb-Hashemi H (2010) The effect of the frontal plane tibiofemoral angle and varus knee moment on the contact stress and strain at the knee cartilage. J Appl Biomech 26:432–443
Yang NH, Nayeb-Hashemi H, Canavan PK, Vaziri A (2010) Effect of frontal plane tibiofemoral angle on the stress and strain at the knee cartilage during the stance phase of gait. J Orthop Res 28:1539–1547
Author information
Authors and Affiliations
Contributions
AB, UGL, AN and VD contributed to the conception and design of the work. AB, GS, AO, JE, JD, AR and AN contributed to acquisition, of data. AB, GS, JE, AN, JD, AR and UGL contributed to analysis and interpretation of data for the work, AB, UGL, AN and VD drafted the work and revised it critically for important intellectual content. Final approval of the version to be published was obtained from all authors. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Funding
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or non-for-profit sectors.
Ethical approval
Institutional Review Board (IRB) approvals are not required for cadaveric studies at the institution. The cadaveric specimens were obtained from an anatomic tissue provider for research, operating according to ethical guidelines associated with the use of such specimens for research purposes. The specimens were received in a de-identified state.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Berton, A., Salvatore, G., Nazarian, A. et al. Combined MPFL reconstruction and tibial tuberosity transfer avoid focal patella overload in the setting of elevated TT–TG distances. Knee Surg Sports Traumatol Arthrosc 31, 1771–1780 (2023). https://doi.org/10.1007/s00167-022-07056-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-07056-6