Abstract
Purpose
The aim of this study was to evaluate the correlation between tibial tuberosity–trochlear groove distance (TT–TG) and body height or knee size, and to find height-related pathologic thresholds of increased TT–TG.
Methods
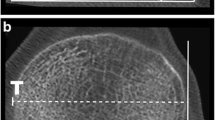
One-hundred and fifty-three patients with recurrent patellar instability and 151 controls were included. The TT–TG was measured on axial computed tomography (CT) images. Femora width and tibial width were selected to represent knee size. The correlation of TT–TG and gender, body height, femora width, and tibial width was evaluated. The height-related pathologic threshold of increased TT–TG was produced according to Dejour’s method. To combine TT–TG with body height and knee size, three new indexes were introduced, ratio of TT–TG to body height (RTH), ratio of TT–TG to femoral width (RTF), and ratio of TT–TG to tibial width (RTT). The ability to predict patellar instability was assessed by the receiver-operating characteristic (ROC) curve, odds ratios (ORs), sensitivity, and specificity.
Results
In patients with patellar instability, TT–TG showed significantly correlation with patient height, femoral width, and tibial width respectively (range r = 0.266–0.283). This correlation was not found in the control group. The pathologic threshold of TT–TG was 18 mm in patients < 169 cm (53%), and the mean TT–TG was 21 mm in patients ≥ 169 cm (54%). There was significant difference in RTH, RTF, and RTT between the two groups. RTH, RTF and RTT have similar large area under the curve (AUC) with TT–TG.
Conclusions
TT–TG showed significant correlation with body height and knee size, respectively. The pathologic threshold of increased TT–TG was suggested to be 21 mm for patients \(\ge\) 169 cm and 18 mm for patients \(<\) 169 cm. Body height-related pathologic threshold provided a supplement for indications of tibial tuberosity medialization.
Level of evidence
IV.


Similar content being viewed by others

References
Bailey M, Metcalfe A, Hing CB, Eldridge J (2021) Consensus guidelines for management of patellofemoral instability. Knee 29:305–312
Balcarek P, Jung K, Frosch KH, Sturmer KM (2011) Value of the tibial tuberosity-trochlear groove distance in patellar instability in the young athlete. Am J Sports Med 39(8):1756–1761
Camp CL, Heidenreich MJ, Dahm DL, Stuart MJ, Levy BA, Krych AJ (2016) Individualizing the tibial tubercle-trochlear groove distance: patellar instability ratios that predict recurrent instability. Am J Sports Med 44(2):393–399
Cao P, Niu Y, Liu C, Wang X, Duan G, Mu Q, Luo X, Wang F (2018) Ratio of the tibial tuberosity-trochlear groove distance to the tibial maximal mediolateral axis: a more reliable and standardized way to measure the tibial tuberosity-trochlear groove distance. Knee 25(1):59–65
Dai ZZ, Sha L, Zhang ZM, Liang ZP, Li H, Li H (2021) Comparing the tibial tuberosity–trochlear groove distance between CT and MRI in skeletally immature patients with and without patellar instability. Orthop J Sports Med 9(1):2325967120973665. https://doi.org/10.1177/2325967120973665
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2(1):19–26
Dornacher D, Reichel H, Kappe T (2016) Does tibial tuberosity-trochlear groove distance (TT–TG) correlate with knee size or body height? Knee Surg Sports Traumatol Arthrosc 24(9):2861–2867
Ferlic PW, Runer A, Dirisamer F, Balcarek P, Giesinger J, Biedermann R, Liebensteiner MC (2018) The use of tibial tuberosity–trochlear groove indices based on joint size in lower limb evaluation. Int Orthop 42(5):995–1000
Hernigou J, Chahidi E, Bouaboula M, Moest E, Callewier A, Kyriakydis T, Koulalis D, Bath O (2018) Knee size chart nomogram for evaluation of tibial tuberosity–trochlear groove distance in knees with or without history of patellofemoral instability. Int Orthop 42(12):2797–2806
Hingelbaum S, Best R, Huth J, Wagner D, Bauer G, Mauch F (2014) The TT–TG Index: a new knee size adjusted measure method to determine the TT–TG distance. Knee Surg Sports Traumatol Arthrosc 22(10):2388–2395
Huntington LS, Webster KE, Devitt BM, Scanlon JP, Feller JA (2020) Factors associated with an increased risk of recurrence after a first-time patellar dislocation: a systematic review and meta-analysis. Am J Sports Med 48(10):2552–2562
Moya-Angeler J, Vairo GL, Bader DA, Sebastianelli WJ, Sherbondy PS (2021) The TT–TG distance/trochlear dysplasia index quotient is the most accurate indicator for determining patellofemoral instability risk. Arthroscopy S0749–8063(21):00770–00772. https://doi.org/10.1016/j.arthro.2021.08.018
Pennock AT, Alam M, Bastrom T (2014) Variation in tibial tubercle-trochlear groove measurement as a function of age, sex, size, and patellar instability. Am J Sports Med 42(2):389–393
Polat AE, Polat B, Gürpınar T, Sarı E, Çarkçı E, Erler K (2020) Tibial tubercle-trochlear groove (TT–TG) distance is a reliable measurement of increased rotational laxity in the knee with an anterior cruciate ligament injury. Knee 27(5):1601–1607
Schoettle PB, Zanetti M, Seifert B, Pfirrmann CW, Fucentese SF, Romero J (2006) The tibial tuberosity–trochlear groove distance; a comparative study between CT and MRI scanning. Knee 13(1):26–31
Su P, Hu H, Li S, Xu T, Li J, Fu W (2022) Tibial tubercle–trochlear groove/trochlear width is the optimal indicator for diagnosing a lateralized tibial tubercle in recurrent patellar dislocation requiring surgical stabilization. Arthroscopy 38(4):1288–1298
Su P, Jian N, Mao B, Zhang Z, Li J, Fu W (2021) Defining the role of TT–TG and TT-PCL in the diagnosis of lateralization of the tibial tubercle in recurrent patellar dislocation. BMC Musculoskelet Disord 22(1):52. https://doi.org/10.1186/s12891-020-03900-3
Tan S, Lim BY, Chng K, Doshi C, Wong F, Lim A, Hui JH (2020) The Difference between computed tomography and magnetic resonance imaging measurements of tibial tubercle–trochlear groove distance for patients with or without patellofemoral instability: a systematic review and meta-analysis. J Knee Surg 33(8):768–776
White AE, Otlans PT, Horan DP, Calem DB, Emper WD, Freedman KB, Tjoumakaris FP (2021) Radiologic measurements in the assessment of patellar instability: a systematic review and meta-analysis. Orthop J Sports Med 9(5):1813040603. https://doi.org/10.1177/2325967121993179
Funding
This work was supported by the National Natural Science Foundation of China (Grant Nos. 51773004, 81630056, 51920105006, 51803188, and 31670982) and National Key Research and Development Program (Grant No. 2016YFC1100704).
Author information
Authors and Affiliations
Contributions
Conception and design of the study: H-JW. Acquisition of data: Y-FS, YM, LL, and JW. Analysis, or interpretation of data: Y-JW, YL, and WL. Drafting the work: H-JW and Y-FS. Revising it critically for important intellectual content: J-KY and FW. Final approval of the version to be published: H-JW, Y-FS, YM, LL, JW, Y-JW, YL, WL, FW, and J-KY. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: H-JW, Y-FS, YM, LL, JW, Y-JW, YL, WL, FW, and J-KY.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the ethics committee of Peking University Third Hospital. (Project Number: 2014099).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, HJ., Song, YF., Ma, Y. et al. Higher pathologic threshold of increased tibial tuberosity–trochlear groove distance should be considered for taller patients. Knee Surg Sports Traumatol Arthrosc 30, 3760–3766 (2022). https://doi.org/10.1007/s00167-022-06992-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-06992-7