Abstract
Purpose
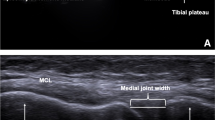
The coronal lateral collateral ligament (LCL) sign has been reported to be associated with deviated position of the tibia on MRI due to anterior cruciate ligament (ACL) injuries. However, the relationships between LCL sign and clinical knee laxity evaluations are still unclear. The purpose of the study was to investigate the relationship between the coronal LCL sign and knee laxity measurements.
Methods
A retrospective review of unilateral ACL injured patients who underwent ACL reconstruction was performed. The coronal LCL sign was determined using magnetic resonance imaging (MRI). Clinical grading of the pivot-shift test, KT-1000 measurements, and quantitative measurements of the Lachman test and the pivot-shift test using an electromagnetic system, were compared between patients with positive and negative coronal LCL sign. A subgroup analysis of different age groups was then performed, dividing patients to adolescent (age ≤ 18 years) and adult (age > 18 years) groups.
Results
A total of 85 patients were enrolled, of which 45 patients had coronal LCL signs. The coronal LCL sign was not associated with the pivot-shift test clinical grading (n.s), KT-1000 measurement (n.s), the tibial translation during the Lachman test (n.s), or with tibia acceleration (n.s) and translation (n.s) during the pivot-shift test. The subgroup analysis also showed that the aforementioned parameters were not associated with the coronal LCL sign in either adolescent or adult subgroups.
Conclusion
The occurrence of coronal LCL sign in MRI did not imply greater clinical knee laxity evaluations in patients with ACL tears. The knee laxity should routinely be evaluated regardless the coronal LCL sign.
Level of evidence
Level III.


Similar content being viewed by others
References
Araki D, Kuroda R, Kubo S, Nagamune K, Hoshino Y, Nishimoto K et al (2011) The use of an electromagnetic measurement system for anterior tibial displacement during the Lachman test. Arthroscopy 27:792–802
Araki D, Matsushita T, Hoshino Y, Nagai K, Nishida K, Koga H et al (2019) The anterolateral structure of the knee does not affect anterior and dynamic rotatory stability in anterior cruciate ligament injury: quantitative evaluation with the electromagnetic measurement system. Am J Sports Med 47:3381–3388
Ayeni OR, Chahal M, Tran MN, Sprague S (2012) Pivot shift as an outcome measure for ACL reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc 20:767–777
Chang MJ, Chang CB, Choi JY, Je MS, Kim TK (2014) Can magnetic resonance imaging findings predict the degree of knee joint laxity in patients undergoing anterior cruciate ligament reconstruction? BMC Musculoskelet Disord 15:214
Curado J, Hulet C, Hardy P, Jenny JY, Rousseau R, Lucet A et al (2020) Very long-term osteoarthritis rate after anterior cruciate ligament reconstruction: 182 cases with 22-year’ follow-up. Orthop Traumatol Surg Res 106:459–463
Galway HR, MacIntosh DL (1980) The lateral pivot shift: a symptom and sign of anterior cruciate ligament insufficiency. Clin Orthop Relat Res 2:45–50
Grassi A, Pizza N, Al-Zu’bi BBH, Fabbro GD, Lucidi GA, Zaffagnini S (2022) Clinical outcomes and osteoarthritis at very long-term follow-up after acl reconstruction: a systematic review and meta-analysis. Orthop J Sports Med 10:23259671211062240
Grood ES, Suntay WJ (1983) A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng 105:136–144
Hardy A, Klouche S, Szarzynski P, Charpentier E, Beranger JS, Bauer T et al (2019) A threshold value of 3.5 mm of passive anterior tibial subluxation on MRI is highly specific for complete ACL tears. Knee Surg Sports Traumatol Arthrosc 27:885–892
Hiroshima Y, Hoshino Y, Miyaji N, Tanaka T, Araki D, Kanzaki N et al (2020) No difference in postoperative rotational laxity after ACL reconstruction in patients with and without anterolateral capsule injury: quantitative evaluation of the pivot-shift test at 1-year follow-up. Knee Surg Sports Traumatol Arthrosc 28:489–494
Hoshino Y, Hiroshima Y, Miyaji N, Nagai K, Araki D, Kanzaki N et al (2020) Unrepaired lateral meniscus tears lead to remaining pivot-shift in ACL-reconstructed knees. Knee Surg Sports Traumatol Arthrosc 28:3504–3510
Hoshino Y, Kuroda R, Nagamune K, Araki D, Kubo S, Yamaguchi M et al (2012) Optimal measurement of clinical rotational test for evaluating anterior cruciate ligament insufficiency. Knee Surg Sports Traumatol Arthrosc 20:1323–1330
Hoshino Y, Kuroda R, Nagamune K, Yagi M, Mizuno K, Yamaguchi M et al (2007) In vivo measurement of the pivot-shift test in the anterior cruciate ligament-deficient knee using an electromagnetic device. Am J Sports Med 35:1098–1104
Hoshino Y, Miyaji N, Nishida K, Nishizawa Y, Araki D, Kanzaki N et al (2019) The concomitant lateral meniscus injury increased the pivot shift in the anterior cruciate ligament-injured knee. Knee Surg Sports Traumatol Arthrosc 27:646–651
Irrgang JJ, Ho H, Harner CD, Fu FH (1998) Use of the International Knee Documentation Committee guidelines to assess outcome following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 6:107–114
James SL, Connell DA (2006) The vertically orientated fibular collateral ligament: a secondary sign of anterior cruciate ligament rupture on magnetic resonance imaging. Eur Radiol 16:1854–1856
Jonsson H, Riklund-Ahlstrom K, Lind J (2004) Positive pivot shift after ACL reconstruction predicts later osteoarthrosis: 63 patients followed 5–9 years after surgery. Acta Orthop Scand 75:594–599
Kaeding CC, Leger-St-Jean B, Magnussen RA (2017) Epidemiology and diagnosis of anterior cruciate ligament injuries. Clin Sports Med 36:1–8
Keizer MNJ, Hijmans JM, Gokeler A, Benjaminse A, Otten E (2020) Healthy subjects with lax knees use less knee flexion rather than muscle control to limit anterior tibia translation during landing. J Exp Orthop 7:32
Kocher MS, Steadman JR, Briggs K, Zurakowski D, Sterett WI, Hawkins RJ (2002) Determinants of patient satisfaction with outcome after anterior cruciate ligament reconstruction. J Bone Joint Surg Am 84:1560–1572
Kono Y, Deie M, Fujita N, Hirata K, Shimada N, Orita N et al (2019) The relationship between knee biomechanics and clinical assessments in ACl deficient patients. Int J Sports Med 40:477–483
Magnussen RA, Reinke EK, Huston LJ, Group MK, Hewett TE, Spindler KP et al (2018) Effect of high-grade preoperative knee laxity on 6-year anterior cruciate ligament reconstruction outcomes. Am J Sports Med 46:2865–2872
Markolf KL, Du PZ, McAllister DR (2021) Changes in knee kinematics from applied external tibial torque: implications for stabilizing an anterior cruciate ligament deficient knee. Clin Biomech 81:105230
Mitchell BC, Siow MY, Bastrom T, Bomar JD, Pennock AT, Parvaresh K et al (2021) Coronal lateral collateral ligament sign: a novel magnetic resonance imaging sign for identifying anterior cruciate ligament-deficient knees in adolescents and summarizing the extent of anterior tibial translation and femorotibial internal rotation. Am J Sports Med 49:928–934
Mitchell BC, Siow MY, Bastrom T, Bomar JD, Pennock AT, Parvaresh K et al (2021) Predictive value of the magnetic resonance imaging-based coronal lateral collateral ligament sign on adolescent anterior cruciate ligament reconstruction graft failure. Am J Sports Med 49:935–940
Miyaji N, Hoshino Y, Tanaka T, Nishida K, Araki D, Kanzaki N et al (2019) MRI-determined anterolateral capsule injury did not affect the pivot-shift in anterior cruciate ligament-injured knees. Knee Surg Sports Traumatol Arthrosc 27:3426–3431
Murphy BJ, Smith RL, Uribe JW, Janecki CJ, Hechtman KS, Mangasarian RA (1992) Bone signal abnormalities in the posterolateral tibia and lateral femoral condyle in complete tears of the anterior cruciate ligament: a specific sign? Radiology 182:221–224
Musahl V, Karlsson J (2019) Anterior cruciate ligament tear. N Engl J Med 380:2341–2348
Nagai K, Hoshino Y, Nishizawa Y, Araki D, Matsushita T, Matsumoto T et al (2015) Quantitative comparison of the pivot shift test results before and after anterior cruciate ligament reconstruction by using the three-dimensional electromagnetic measurement system. Knee Surg Sports Traumatol Arthrosc 23:2876–2881
Ng WH, Griffith JF, Hung EH, Paunipagar B, Law BK, Yung PS (2011) Imaging of the anterior cruciate ligament. World J Orthop 2:75–84
Nishida K, Matsushita T, Hoshino Y, Araki D, Matsumoto T, Niikura T et al (2020) The influences of chronicity and meniscal injuries on pivot shift in anterior cruciate ligament-deficient knees: quantitative evaluation using an electromagnetic measurement system. Arthroscopy 36:1398–1406
Numkarunarunrote N, Chaitusaney T (2015) Anterior tibial translation sign: factors affecting interpretation of anterior cruciate ligament tear. J Med Assoc Thai 98(Suppl 1):S57-62
Pao DG (2001) The lateral femoral notch sign. Radiology 219:800–801
Pringle L, Wissman R (2021) Imaging of noncontact anterior cruciate ligament injuries and associated bone marrow contusion patterns. J Knee Surg. https://doi.org/10.1055/s-0041-1740393
Singh H, McKay M, Baldwin J, Nicholson L, Chan C, Burns J et al (2017) Beighton scores and cut-offs across the lifespan: cross-sectional study of an Australian population. Rheumatology (Oxford) 56:1857–1864
Tanaka T, Hoshino Y, Miyaji N, Ibaragi K, Nishida K, Nishizawa Y et al (2018) The diagnostic reliability of the quantitative pivot-shift evaluation using an electromagnetic measurement system for anterior cruciate ligament deficiency was superior to those of the accelerometer and iPad image analysis. Knee Surg Sports Traumatol Arthrosc 26:2835–2840
Terzidis IP, Christodoulou AG, Ploumis AL, Metsovitis SR, Koimtzis M, Givissis P (2004) The appearance of kissing contusion in the acutely injured knee in the athletes. Br J Sports Med 38:592–596
Ueki H, Nakagawa Y, Ohara T, Watanabe T, Horie M, Katagiri H et al (2018) Risk factors for residual pivot shift after anterior cruciate ligament reconstruction: data from the MAKS group. Knee Surg Sports Traumatol Arthrosc 26:3724–3730
Vassalou EE, Klontzas ME, Kouvidis GK, Matalliotaki PI, Karantanas AH (2016) Rotational knee laxity in anterior cruciate ligament deficiency: an additional secondary sign on MRI. AJR Am J Roentgenol 206:151–154
Yamamoto Y, Tsuda E, Maeda S, Naraoka T, Kimura Y, Chiba D et al (2018) Greater laxity in the anterior cruciate ligament-injured knee carries a higher risk of postreconstruction pivot shift: intraoperative measurements with a navigation system. Am J Sports Med 46:2859–2864
Funding
The authors report no involvement in the research by the sponsor that could have influenced the outcome of this work.
Author information
Authors and Affiliations
Contributions
CKH, YH and SW have given substantial contributions to conception, performance of work and preparation of the manuscript. KN, TM, WRS and RK have given substantial contributions to performance of work and interpretation or analysis of data. All authors have participated to revision for important intellectual content. CKH and YH revised it critically and provided supervision with this study. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
Ethical considerations
All the participants understood the purpose of this study and provided informed consent prior to participation according to the ethical standards of the Declaration of Helsinki, and this research was conducted with the approval of Kobe University Ethics Committee (No. B190055).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hong, CK., Hoshino, Y., Watanabe, S. et al. The coronal lateral collateral ligament sign in the anterior cruciate ligament-injured knees was observed regardless of the knee laxity based on the quantitative measurements. Knee Surg Sports Traumatol Arthrosc 30, 3508–3514 (2022). https://doi.org/10.1007/s00167-022-06970-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-06970-z