Abstract
Purpose
The purpose of this study was to determine the effect of obesity on patient outcome, procedure failure rate and osteoarthritis (OA) progression in the tibiofemoral compartments in a series of isolated patellofemoral arthroplasty (PFA) performed with a third-generation implant.
Methods
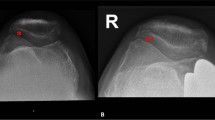
The study population was patients who had undergone third-generation PFA at a specialized orthopedic center between 2007 and 2017. Patients were categorized by body-mass index (BMI) as obese (O, BMI > 30 kg/m2) or nonobese (NO, BMI < 30 kg/m2). Preoperative and postoperative clinical and functional assessment included knee range of motion, Knee Society Score (KSS), University of California Los Angeles (UCLA) Activity Score, Tegner Activity Level Scale, and visual analogue scale (VAS) for pain. Preoperative and postoperative radiographs were evaluated for progression of tibiofemoral compartment OA, changes in patellar height and in knee coronal alignment. Multiple logistic regression models were used to assess the effect of BMI on outcomes together with other covariates.
Results
A total of 120 PFAs with a mean follow-up of 6.9 ± 2.5 years were included: 25 in the O group and 95 in the NO group. Significant improvement was noted in in knee range of motion (P < 0.001), clinical and functional KSS (P < 0.001), UCLA Activity Score (P < 0.001), Tegner score (P < 0.001) and VAS pain (P < 0.001) without inter-groups differences. Worsening of the medial Kellgren–Lawrence (KL) grade (but not the lateral KL grade) was more frequent in the O than the NO group during the follow-up period (P = 0.014). Failure occurred in 4.2% of NO and in 20% of O group patients; the difference was solely due to failure because of OA progression in the tibiofemoral compartment (16% in the O group). There were no between group differences in the failure rate for any cause other than OA progression (4.2% in the NO group, 4.0% in the O group).
Conclusions
An equal improvement in function after PFA was noted in both obese and nonobese patients; however, the high failure rate due to OA progression in the medial tibiofemoral compartment warrants caution when considering PFA in obese patients.

Similar content being viewed by others
Abbreviations
- PFA:
-
Patellofemoral arthroplasty
- TKA:
-
Total knee arthroplasty
- OA:
-
Osteoarthritis
- ROM:
-
Range of motion
- BMI:
-
Body mass index
- VAS:
-
Visual analogue scale
- KL:
-
Kellgren–Lawrence
- KSS:
-
Knee Society score
- UCLA:
-
University of California Los Angeles Activity Score
- HKA:
-
Hip–knee–ankle angle
- O:
-
Obese
- NO:
-
Non obese
- OR:
-
Odds ratio
References
Ackerman IN, Kemp JL, Crossley KM, Culvenor AG, Hinman RS (2017) Hip and knee osteoarthritis affects younger people, too. J Orthop Sports Phys Ther 47:67–79
Bunyoz KI, Lustig S, Troelsen A (2019) Similar postoperative patient-reported outcome in both second generation patellofemoral arthroplasty and total knee arthroplasty for treatment of isolated patellofemoral osteoarthritis: a systematic review. Knee Surg Sports Traumatol Arthrosc 27(7):2226–2237
Caton J, Deschamps G, Chambat P, Lerat JL, Dejour H (1982) Patella infera. A propos of 128 cases. Rev Chir Orthop Reparatrice Appar Mot 68:317–325
Chaudhry H, Ponnusamy K, Somerville L, McCalden RW, Marsh J, Vasarhelyi EM (2019) Revision rates and functional outcomes among severely, morbidly, and super-obese patients following primary total knee arthroplasty: a systematic review and meta-analysis. JBJS Rev 7:e9. https://doi.org/10.2106/JBJS.RVW.18.00184
Dahm DL, Al-Rayashi W, Dajani K, Shah JP, Levy BA, Stuart MJ (2010) Patellofemoral arthroplasty versus total knee arthroplasty in patients with isolated patellofemoral osteoarthritis. Am J Orthop 39:487–491
Dahm DL, Kalisvaart MM, Stuart MJ, Slettedahl SW (2014) Patellofemoral arthroplasty: outcomes and factors associated with early progression of tibiofemoral arthritis. Knee Surg Sports Traumatol Arthrosc 22:2554–2559
Dejour D, Reynaud P, Lecoultre B (1998) Douleurs et instabilite rotulienne, essai de classification. Med Hyg 56:1466–1471
Desai VS, Pareek A, DeDeugd CM, Sabbag OD, Krych AJ, Cummings NM, Dahm DL (2020) Smoking, unemployment, female sex, obesity, and medication use yield worse outcomes in patellofemoral arthroplasty. Knee Surg Sports Traumatol Arthrosc 28:2962–2969
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the knee society clinical rating system. Clin Orthop Relat Res 248:13–14
Iwano T, Kurosawa H, Tokuyama H, Hoshikawa Y (1990) Roentgenographic and clinical findings of patellofemoral osteoarthrosis: with special reference to its relationship to femorotibial osteoarthrosis and etiologic factors. Clin Orthop 252:190–197
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteoarthrosis. Ann Rheum Dis 16:494–502
Liow MH, Goh GS, Tay DK, Chia SL, Lo NN, Yeo SJ (2016) Obesity and the absence of trochlear dysplasia increase the risk of revision in patellofemoral arthroplasty. Knee 23(2):331–337
Onggo JR, Onggo JD, de Steiger R, Hau R (2020) Greater risks of complications, infections, and revisions in the obese versus non-obese total hip arthroplasty population of 2,190,824 patients: a meta-analysis and systematic review. Osteoarthr Cartil 28(1):31–44
Romagnoli S, Marullo M (2018) Mid-term clinical, functional, and radiographic outcomes of 105 gender-specific patellofemoral arthroplasties, with or without the association of medial unicompartmental knee arthroplasty. J Arthroplasty 33:688–695
Schneider BL, Ling DI, Kleebad LJ, Strickland S, Pearle A (2020) Comparing return to sports after patellofemoral and knee arthroplasty in an age- and sex- matched cohort. Orthop J Sports Med 5(8):2325967120957425
Tegner Y, Lysholm J (1995) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Tillman MD, Smith KR, Bauer JA, Cauraugh JH, Falsetti AB, Pattishall JL (2002) Differences in three intercondylar notch geometry indices between males and females: a cadaveric study. Knee 9:41–46
Tishelman JC, Pyne A, Kahlenberg CA, Gruskay JA, Strickland SM (2020) Obesity does not affect patient-reported outcomes following patellofemoral arthroplasty. J Knee Surg. https://doi.org/10.1055/s-0040-1713862
van der List JP, Chawla H, Villa JC, Pearle AD (2017) Why do patellofemoral arthroplasties fail today? A systematic review. Knee 24(1):2–8
van der List JP, Chawla H, Zuiderbaan HA, Pearle AD (2017) Survivorship and functional outcomes of patellofemoral arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc 25(8):2622–2631
van Jonbergen HP, Werkman DM, Barnaart LF, van Kampen A (2010) Long-term outcomes of patellofemoral arthroplasty. J Arthroplasty 25:1066–1071
Vandenneucker H, Labey L, Vander Sloten J, Desloovere K, Bellemans J (2016) Isolated patellofemoral arthroplasty reproduces natural patellofemoral joint kinematics when the patella is resurfaced. Knee Surg Sports Traumatol Arthrosc 24:3668–3677
Varadarajan KM, Gill TJ, Freiberg AA, Rubash HE, Li G (2009) Gender differences in trochlear groove orientation and rotational kinematics of human knees. J Orthop Res 27:871–878
Vasso M, Corona K, Gomberg B, Marullo M, European Knee Associates Small Implants focus group (2021) Obesity increases the risk of conversion to total knee arthroplasty after unicompartimental knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06780-9
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP et al (2014) The strengthening the reporting of observational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg 12:1495–1499
Wiberg G (1941) Roentgenographic and anatomic studies on the patellofemoral joint with special reference to chondromalacia patellae. Acta Orthop Scand 12:319–410
Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC (1998) Assessing activity in joint replacement patients. J Arthroplasty 13:890–895
Zheng H, Chen C (2015) Body mass index and risk of knee osteoarthritis: systematic review and meta-analysis of prospective studies. BMJ Open 5(12):e007568
Funding
None.
Author information
Authors and Affiliations
Contributions
MM was involved with study design, data collection, drafting, editing and reviewing of the manuscript; MB was involved with drafting and reviewing of the manuscript. CL was involved with data collection and drafting of the manuscript. MV was involved with statistical analysis, drafting, editing and reviewing of the manuscript. SR was involved with drafting and reviewing of the manuscript. All contributors met the ICMJE and journal criteria for authorship and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Romagnoli is a paid consultant and receives royalties from Zimmer Biomet. The other authors reported no conflict of interest.
Ethical approval
The study was approved by the Ethical Committee of the IRCCS Ospedale San Raffaele (reference number: 134/INT/2017).
Informed consent
Informed consent was obtained from all the participants who were included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Marullo, M., Bargagliotti, M., Vigano’, M. et al. Patellofemoral arthroplasty: obesity linked to high risk of revision and progression of medial tibiofemoral osteoarthritis. Knee Surg Sports Traumatol Arthrosc 30, 4115–4122 (2022). https://doi.org/10.1007/s00167-022-06947-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-06947-y