Abstract
Purpose
To compare the long-term clinical efficacy provided by intra-articular injections of either Pure Platelet-rich Plasma (P-PRP) or sham saline to treat knee osteoarthritis (KOA).
Methods
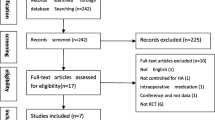
This prospective, parallel-group, double-blind, multi-center, sham-controlled randomized clinical trial recruited participants with KOA from orthopedic departments at nine public hospitals (five tertiary medical centers, four secondary medical units) starting January 1, 2014, with follow-up completed on February 28, 2021. Participants were randomly allocated to interventions in a 1:1 ratio. Data were analyzed from March 1, 2021, to July 15, 2021. Three sessions (1 every week) of P-PRP or sham saline injected by physicians. The primary outcome was the Western Ontario and McMaster Universities Arthritis Index (WOMAC) at 3, 6, 12, 24, 60 months of follow-up. Secondary outcomes included the International Knee Documentation Committee (IKDC) subjective score, visual analogue scale (VAS) score, intra-articular biochemical marker concentrations, cartilage volume, and adverse events. Laboratory of each hospital analyzed the content and quality of P-PRP.
Results
610 participants (59% women) with KOA who received three sessions of P-PRP (n = 308, mean age 53.91 years) or sham saline (n = 302, mean age 54.51 years) injections completed the trial. The mean platelet concentration in PRP is 4.3fold (95% confidence interval 3.6–4.5) greater than that of whole blood. Both groups showed significant improvements in IKDC, WOMAC, and VAS scores at 1 month of follow-up. However, only the P-PRP group showed a sustained improvement in clinical outcome measurements at month 24 (P < 0.001). There were statistically significant differences between the P-PRP and sham saline groups in all clinical outcome measurements at each follow-up time point (P < 0.001). The benefit of P-PRP was clinically better in terms of WOMAC-pain, WOMAC-physical function and WOMAC-total at 6, 12, 24, and 60 months of follow-up. No clinically significant differences between treatments were documented in terms of WOMAC-stiffness at any follow-up. A clinically significant difference favoring P-PRP group against saline in terms of IKDC and VAS scores was documented at 6, 12, 24 and 60 months of follow-up. At 6 months after injection, TNF-α and IL-1β levels in synovial fluid were lower in the P-PRP group (P < 0.001). Tibiofemoral cartilage volume decreased by a mean value of 1171 mm3 in the P-PRP group and 2311 mm3 in the saline group over 60 months and the difference between the group was statistically significant (intergroup difference, 1140 mm3, 95% CI − 79 to 1320 mm3; P < 0.001).
Conclusions
In this randomized clinical trial of patients with KOA, P-PRP was superior to sham saline in treating KOA. P-PRP was effective for achieving at least 24 months of symptom relief and slowing the progress of KOA, with both P-PRP and saline being comparable in safety profiles.


Similar content being viewed by others
References
Angst F, Aeschlimann A, Stucki G (2001) Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF-36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities. Arthritis Rheum 45(4):384–391
Boffa A, Salerno M, Merli G et al (2021) Platelet-rich plasma injections induce disease-modifying effects in the treatment of osteoarthritis in animal models. Knee Surg Sports Traumatol Arthrosc 29(12):4100–4121
Castillo TN, Pouliot MA, Kim HJ, Dragoo JL (2011) Comparison of growth factor and platelet concentration from commercial platelet-rich plasma separation systems. Am J Sports Med 39(2):266–271
Cicuttini FM, Jones G, Forbes A, Wluka AE (2004) Rate of cartilage loss at two years predicts subsequent total knee arthroplasty: a prospective study. Ann Rheum Dis 63(9):1124–1127
Cole BJ, Karas V, Hussey K, Pilz K, Fortier LA (2017) Hyaluronic acid versus platelet-rich plasma: a prospective, double-blind randomized controlled trial comparing clinical outcomes and effects on intra-articular biology for the treatment of knee osteoarthritis. Am J Sports Med 45(2):339–346
Dai WL, Zhou AG, Zhang H, Zhang J (2017) Efficacy of platelet-rich plasma in the treatment of knee osteoarthritis: a meta-analysis of randomized controlled trials. Arthroscopy 33(3):659-670.e651
Di Martino A, Di Matteo B, Papio T et al (2019) Platelet-rich plasma versus hyaluronic acid injections for the treatment of knee osteoarthritis: results at 5 years of a double-blind, randomized controlled trial. Am J Sports Med 47(2):347–354
Duymus TM, Mutlu S, Dernek B, Komur B, Aydogmus S, Kesiktas FN (2017) Choice of intra-articular injection in treatment of knee osteoarthritis: platelet-rich plasma, hyaluronic acid or ozone options. Knee Surg Sports Traumatol Arthrosc 25(2):485–492
Filardo G, Kon E, Buda R et al (2011) Platelet-rich plasma intra-articular knee injections for the treatment of degenerative cartilage lesions and osteoarthritis. Knee Surg Sports Traumatol Arthrosc 19(4):528–535
Filardo G, Kon E, Roffi A, Di Matteo B, Merli ML, Marcacci M (2015) Platelet-rich plasma: why intra-articular? A systematic review of preclinical studies and clinical evidence on PRP for joint degeneration. Knee Surg Sports Traumatol Arthrosc 23(9):2459–2474
Gobbi A, Lad D, Karnatzikos G (2015) The effects of repeated intra-articular PRP injections on clinical outcomes of early osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc 23(8):2170–2177
Hart R, Safi A, Komzak M, Jajtner P, Puskeiler M, Hartova P (2013) Platelet-rich plasma in patients with tibiofemoral cartilage degeneration. Arch Orthop Trauma Surg 133(9):1295–1301
Irrgang JJ, Anderson AF, Boland AL et al (2001) Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med 29(5):600–613
Laudy AB, Bakker EW, Rekers M et al (2015) Efficacy of platelet-rich plasma injections in osteoarthritis of the knee: a systematic review and meta-analysis. Br J Sports Med 49(10):657–672
Roos EM, Lohmander LS (2003) The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes 1:64
Saltzman BM, Leroux T, Meyer MA et al (2017) The therapeutic effect of intra-articular normal saline injections for knee osteoarthritis: a meta-analysis of evidence level 1 studies. Am J Sports Med 45(11):2647–2653
Xue Y, Su X, Jiang M et al (2020) Pure platelet-rich plasma facilitates the repair of damaged cartilage and synovium in a rabbit hemorrhagic arthritis knee model. Arthritis Res Ther 22(1):68
Yan R, Gu Y, Ran J et al (2017) Intratendon delivery of leukocyte-poor platelet-rich plasma improves healing compared with leukocyte-rich platelet-rich plasma in a rabbit achilles tendinopathy model. Am J Sports Med 45(8):1909–1920
Acknowledgements
The authors thank Dr. Pingcheng Xu from Department of Orthopedics, Wujiang Fourth People’s Hospital, Wujiang, Suzhou; Dr Hao Xu from Department of Orthopedics, Wujiang Second People’s Hospital, Wujiang, Suzhou; Dr Qinghua Zhu from Department of Orthopedics, Wuxi Eighth People’s Hospital, Wuxi, China; Dr. Weili Fu from Department of Orthopedics, West China Hospital, Sichuan University, Chengdu, China; for their help in the study.
Funding
Funding was provided by National Natural Science Foundation of China (Grant no 81201421), National Clinical Research Center for Orthopedics, Sports Medicine & Rehabilitation and Jiangsu China-Israel Industrial Technical Research Institute Foundation (2021-NCRC-CXJJ-PY-09).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
All of the participants provided written informed consent before this study, and the study was approved by the Local Ethics Committee, the First Affiliated Hospital of Soochow University (2013-098).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chu, J., Duan, W., Yu, Z. et al. Intra-articular injections of platelet-rich plasma decrease pain and improve functional outcomes than sham saline in patients with knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc 30, 4063–4071 (2022). https://doi.org/10.1007/s00167-022-06887-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-06887-7