Abstract
Purpose
The purpose of this study was to assess complications, reoperations, and their risk factors at 90 days and 2 years after high tibial osteotomy (HTO) and distal femoral osteotomy (DFO) in a national cohort.
Methods
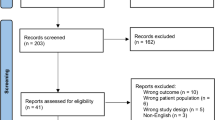
The PearlDiver Mariner Dataset was queried using International Classification of Diseases (ICD) and Current Procedural Terminology (CPT) codes for HTO and DFO, complications, and subsequent surgery. Minimum follow-up was 2 years and complications were assessed at 90 days and 2 years. Hospital readmission in the first 90 days was also assessed. Univariate and multiple logistic regression were utilized to identify risk factors for complications and re-operation.
Results
The 90-day and 2-year complication rates after HTO (n = 1780) were 11.6% and 31.7%, compared to 21.5% (p < 0.0001) and 41.5% (p = 0.0001) after DFO (n = 446). Infection was the most frequent early (90-day) complication for both HTO and DFO cohorts, while hardware problems were most common at 2 years. Increasing Elixhauser Comorbidity Index (ECI) was associated with increased odds of infection, readmission, and hardware-associated complications in both cohorts. Gender and tobacco use were also associated with various complications after HTO. At 2 years, 23.7% of HTO patients and 26.2% of DFO patients had undergone subsequent surgery. Hardware removal occurred in 16.4% of HTO and 18.4% of DFO patients (n.s.), while 4.5% of HTO and 5.2% of DFO patients underwent total knee arthroplasty (TKA) within 2 years (n.s.).
Conclusion
HTO and DFO have substantial complication rates in the short and mid term, with a higher rate of overall complications observed after DFO as compared to the HTO cohort. After both procedures, roughly one quarter of patients will undergo subsequent surgery within 2 years. Patients with tobacco use and numerous medical co-morbidities may not be optimal candidates due to increased complication rates. Elixhauser Comorbidity Index (ECI) may be an useful tool for risk assessment prior to surgery.
Level of evidence
Retrospective cohort study, III.
Similar content being viewed by others
References
Bouguennec N, Mergenthaler G, Gicquel T, Briand C, Nadau E, Pailhé R, Hanouz JL, Fayard JM, Rochcongar G, Francophone Arthroscopy Society (2020) Medium-term survival and clinical and radiological results in high tibial osteotomy: factors for failure and comparison with unicompartmental arthroplasty. Orthop Traumatol Surg Res 106:S223–S230
Brinkman J-M, Lobenhoffer P, Agneskirchner JD, Staubli AE, Wymenga AB, van Heerwaarden RJ (2008) Osteotomies around the knee. J Bone Jt Surg Br 90-B:1548–1557
Brown NM, Sheth NP, Davis K, Berend ME, Lombardi AV, Berend KR, Della Valle CJ (2012) Total knee arthroplasty has higher postoperative morbidity than unicompartmental knee arthroplasty: a multicenter analysis. J Arthroplasty 27:86–90
Cameron JI, McCauley JC, Kermanshahi AY, Bugbee WD (2015) Lateral opening-wedge distal femoral osteotomy: pain relief, functional improvement, and survivorship at 5 years. Clin Orthop Relat Res 473:2009–2015
Cao Z, Mai X, Wang J, Feng E, Huang Y (2018) Unicompartmental knee arthroplasty vs high tibial osteotomy for knee osteoarthritis: a systematic review and meta-analysis. J Arthroplasty 33:952–959
Chahla J, Mitchell JJ, Liechti DJ, Moatshe G, Menge TJ, Dean CS, LaPrade RF (2016) Opening- and closing-wedge distal femoral osteotomy: a systematic review of outcomes for isolated lateral compartment osteoarthritis. Orthop J Sports Med 4(6):2325967116649901
Cotter EJ, Gowd AK, Bohl DD, Getgood A, Cole BJ, Frank RM (2020) Medical comorbidities and functional dependent living are independent risk factors for short-term complications following osteotomy procedures about the knee. Cartilage 11:423–430
Day M, Wolf BR (2019) Medial opening-wedge high tibial osteotomy for medial compartment arthrosis/overload. Clin Sports Med 38:331–349
Delva ML, Samuel LT, Roth A, Yalçin S, Kamath AF (2021) Contemporary knee osteotomy in the united states: high tibial osteotomy and distal femoral osteotomy have comparable complication rates despite differing demographic profiles. J Knee Surg 34:816–821
Duchman KR, Gao Y, Pugely AJ, Martin CT, Callaghan JJ (2014) Differences in short-term complications between unicompartmental and total knee arthroplasty: a propensity score matched analysis. J Bone Jt Surg Am 96:1387–1394
Duivenvoorden T, van Diggele P, Reijman M, Bos PK, van Egmond J, Bierma-Zeinstra SMA, Verhaar JAN (2017) Adverse events and survival after closing- and opening-wedge high tibial osteotomy: a comparative study of 412 patients. Knee Surg Sports Traumatol Arthrosc 25:895–901
Erickson BJ, Tilton A, Frank RM, Park W, Cole BJ (2017) Rates of deep vein thrombosis occurring after osteotomy about the knee. Am J Orthop (Belle Mead NJ) 46:E23–E27
Floerkemeier S, Staubli AE, Schroeter S, Goldhahn S, Lobenhoffer P (2014) Does obesity and nicotine abuse influence the outcome and complication rate after open-wedge high tibial osteotomy? A retrospective evaluation of five hundred and thirty three patients. Int Orthop 38:55–60
Han S-B, In Y, Oh KJ, Song KY, Yun ST, Jang K-M (2019) Complications associated with medial opening-wedge high tibial osteotomy using a locking plate: a multicenter study. J Arthroplasty 34:439–445
Hansen EN, Ong KL, Lau E, Kurtz SM, Lonner JH (2019) Unicondylar knee arthroplasty has fewer complications but higher revision rates than total knee arthroplasty in a study of large united states databases. J Arthroplasty 34:1617–1625
van Houten AH, Heesterbeek PJC, van Heerwaarden RJ, van Tienen TG, Wymenga AB (2014) Medial open wedge high tibial osteotomy: can delayed or nonunion be predicted? Clin Orthop 472:1217–1223
Kawata M, Jo T, Taketomi S, Inui H, Yamagami R, Matsui H, Fushimi K, Yasunaga H, Tanaka S (2021) Type of bone graft and primary diagnosis were associated with nosocomial surgical site infection after high tibial osteotomy: analysis of a national database. Knee Surg Sports Traumatol Arthrosc 29:429–436
Kim C-Y, Sivasundaram L, LaBelle MW, Trivedi NN, Liu RW, Gillespie RJ (2018) Predicting adverse events, length of stay, and discharge disposition following shoulder arthroplasty: a comparison of the Elixhauser Comorbidity Measure and Charlson Comorbidity Index. J Shoulder Elb Surg 27:1748–1755
Klek M, Dhawan A (2019) The role of high tibial osteotomy in ACL reconstruction in knees with coronal and sagittal plane deformity. Curr Rev Musculoskelet Med 12:466–471
Liddle AD, Judge A, Pandit H, Murray DW (2014) Adverse outcomes after total and unicompartmental knee replacement in 101 330 matched patients: a study of data from the National Joint Registry for England and Wales. Lancet 384:1437–1445
Martin R, Birmingham TB, Willits K, Litchfield R, LeBel M-E, Giffin JR (2014) Adverse event rates and classifications in medial opening wedge high tibial osteotomy. Am J Sports Med 42(5):1118–1126
Mayfield CK, Bolia IK, Mayer EN, Heidari KS, Heckmann N, Pannell WC, Hill JR, McKnight B, Vangsness CT, Hatch GF, Weber AE (2020) Factors associated with distal femoral osteotomy survivorship: data from the California Office of Statewide Health Planning and Development (OSHPD) Registry. Orthop J Sports Med 8:2325967120951554
Meidinger G, Imhoff AB, Paul J, Kirchhoff C, Sauerschnig M, Hinterwimmer S (2011) May smokers and overweight patients be treated with a medial open-wedge HTO? Risk factors for non-union. Knee Surg Sports Traumatol Arthrosc 19:333–339
Menendez ME, Neuhaus V, van Dijk CN, Ring D (2014) The elixhauser comorbidity method outperforms the Charlson Index in predicting inpatient death after orthopaedic surgery. Clin Orthop 472:2878–2886
Miller BS, Downie B, McDonough EB, Wojtys EM (2009) Complications after medial opening wedge high tibial osteotomy. Arthroscopy 25:639–646
Mina C, Garrett WE, Pietrobon R, Glisson R, Higgins L (2008) High tibial osteotomy for unloading osteochondral defects in the medial compartment of the knee. Am J Sports Med 36:949–955
Niemeyer P, Schmal H, Hauschild O, von Heyden J, Südkamp NP, Köstler W (2010) Open-wedge osteotomy using an internal plate fixator in patients with medial-compartment gonarthritis and varus malalignment: 3-year results with regard to preoperative arthroscopic and radiographic findings. Arthroscopy 26:1607–1616
Nwachukwu BU, McCormick FM, Schairer WW, Frank RM, Provencher MT, Roche MW (2014) Unicompartmental knee arthroplasty versus high tibial osteotomy: United States practice patterns for the surgical treatment of unicompartmental arthritis. J Arthroplasty 29:1586–1589
O’Malley MP, Pareek A, PatrickJ R, Stuart MJ, Krych AJ (2016) Distal femoral osteotomy: lateral opening wedge technique. Arthrosc Tech 5:e725–e730
Ondeck NT, Bohl DD, Bovonratwet P, McLynn RP, Cui JJ, Grauer JN (2018) Discriminative ability of Elixhauser’s comorbidity measure is superior to other comorbidity scores for inpatient adverse outcomes after total hip arthroplasty. J Arthroplasty 33:250–257
Pannell WC, Heidari KS, Mayer EN, Zimmerman K, Heckmann N, McKnight B, Hill JR, Vangsness CT, Hatch GF, Weber AE (2019) High tibial osteotomy survivorship: a population-based study. Orthop J Sports Med 7:2325967119890693
Seo S-S, Kim O-G, Seo J-H, Kim D-H, Kim Y-G, Lee I-S (2016) Complications and short-term outcomes of medial opening wedge high tibial osteotomy using a locking plate for medial osteoarthritis of the knee. Knee Surg Relat Res 28:289–296
Sherman SL, Thompson SF, Clohisy JCF (2018) Distal femoral varus osteotomy for the management of valgus deformity of the knee. J Am Acad Orthop Surg 26:313–324
Shivji FS, Foster A, Risebury MJ, Wilson AJ, Yasen SK (2021) Ten-year survival rate of 89% after distal femoral osteotomy surgery for lateral compartment osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc 29:594–599
Sidhu R, Moatshe G, Firth A, Litchfield R, Getgood A (2020) Low rates of serious complications but high rates of hardware removal after high tibial osteotomy with Tomofix locking plate. Knee Surg Sports Traumatol Arthrosc 29:3361–3367
Song EK, Seon JK, Park SJ, Jeong MS (2010) The complications of high tibial osteotomy. J Bone Jt Surg Br 92-B:1245–1252
Woodacre T, Ricketts M, Evans JT, Pavlou G, Schranz P, Hockings M, Toms A (2016) Complications associated with opening wedge high tibial osteotomy—a review of the literature and of 15 years of experience. Knee 23:276–282
Yabuuchi K, Kondo E, Onodera J, Onodera T, Yagi T, Iwasaki N, Yasuda K (2020) Clinical outcomes and complications during and after medial open-wedge high tibial osteotomy using a locking plate: a 3- to 7-year follow-up study. Orthop J Sports Med 8:2325967120922535
Yapici F, Aykut US, Coskun M, Arslan MC, Merder-Coskun D, Kocabiyik A, Ulu E, Bayhan A, Kaygusuz MA (2020) Complications, additional surgery, and joint survival analysis after medial open-wedge high tibial osteotomy. Orthopedics 43:303–314
Acknowledgements
We acknowledge Scott Ellison for his assistance with the PearlDiver database.
Funding
This research did not receive any specific grant from funding.
Author information
Authors and Affiliations
Contributions
NKK designed the study, collected data, performed statistical analysis, and drafted the manuscript; CA contributed to writing of manuscript; ALZ, CBM, BTF critically revised the manuscript; DAL conceived of and designed the study and critically revised the manuscript.
Ethics declarations
Conflict of interest
DAL consults for Vericel, Inc., receives educational support from Arthrex/Evolution Surgical, receives research support from AOSSM, AANA, and Arthritis Foundation, and is a committee member of AOSSM, AANA, and ORS; BTF serves on the editorial board of JSES and CRMM, holds stock options with Bioniks and Kaliber.ai, and receives research support from NIH, VA, Orthofix, and Stryker; ALZ is a consultant for Stryker and Depuy-Mitek; CBM is a consultant for Stryker, Conmed, and Tornier, receives research support from Aesculap, Samumed, Zimmer, and Conmed and receives royalties from Conmed.
Ethical approval
Not required.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix A
Codes used to define HTO and DFO cohorts
Procedure | Code |
|---|---|
HTO | CPT-27455, CPT-27457, CPT-27705, CPT-27709, ICD-9-P-7727, ICD-10-P-0Q8G0ZZ, ICD-10-P-0Q8G3ZZ, ICD-10-P-0Q8G4ZZ, ICD-10-P-0Q8H0ZZ, ICD-10-P-0Q8H3ZZ, ICD-10-P-0Q8H4Z |
DFO | CPT-27448, CPT-27450, ICD-9-P-7725, ICD-10-P-0Q8B0ZZ, ICD-10-P-0Q8C0ZZ, ICD-10-P-0Q8C3ZZ, ICD-10-P-0Q8C4ZZ, ICD-10-P-0Q8B3ZZ, ICD-10-P-0Q8B4ZZ |
Associated diagnosis | Code |
|---|---|
Knee osteoarthritis | ICD-9-D-71516, ICD-9-D-71526, ICD-9-D-71536, ICD-9-D-71596, ICD-10-D-M1710, ICD-10-D-M175, ICD-10-D-M179, ICD-10-DM170, ICD-10-D-M1711, ICD-10-D-M1712, ICD-10-D-M172, ICD-10-D-M1730, ICD-10-D-M1731, ICD-10-D-M1732, ICD-10-D-M174, ICD-10-D-M175 |
Meniscus tear | ICD-9-D-7170, ICD-9-D-7171, ICD-9-D-7172, ICD-9-D-7173, ICD-9-D-71740, ICD-9-D-71741, ICD-9-D-71742, ICD-9-D-71743, ICD-9-D-71749, ICD-9-D-7175, ICD-9-D-8360, ICD-9-D-8361, ICD-9-D-8362, ICD-10-D-S83252A, ICD-10-D-S83252S, ICD-10-D-S83252D, ICD-10-D-S83251A, ICD-10-D-S83251S, ICD-10-D-S83251D, ICD-10-D-S83259A, ICD-10-D-S83259S, ICD-10-D-S83259D, ICD-10-D-S83212A, ICD-10-D-S83212S, ICD-10-D-S83212D, ICD-10-D-S83211A, ICD-10-D-S83211S, ICD-10-D-S83211D, ICD-10-D-S83219A, ICD-10-D-S83219S, ICD-10-D-S83219D, ICD-10-D-S83201A, ICD-10-D-S83201S, ICD-10-D-S83201D, ICD-10-D-S83200A, ICD-10-D-S83200S, ICD-10-D-S83200D, ICD-10-D-S83202A, ICD-10-D-S83202S, ICD-10-D-S83202D, ICD-10-D-S83272A, ICD-10-D-S83272S, ICD-10-D-S83272D, ICD-10-D-S83271A, ICD-10-D-S83271S, ICD-10-D-S83271D, ICD-10-D-S83279A, ICD-10-D-S83279S, ICD-10-D-S83279D, ICD-10-D-S83232A, ICD-10-D-S83232S, ICD-10-D-S83232D, ICD-10-D-S83231A, ICD-10-D-S83231S, ICD-10-D-S83231D, ICD-10-D-S83239A, ICD-10-D-S83239S, ICD-10-D-S83239D, ICD-10-D-M23242, ICD-10-D-M23241, ICD-10-D-M23249, ICD-10-D-M23212, ICD-10-D-M23211, ICD-10-D-M23219, ICD-10-D-M23262, ICD-10-D-M23261, ICD-10-D-M23269, ICD-10-D-M23232, ICD-10-D-M23231, ICD-10-D-M23239, ICD-10-D-M23252, ICD-10-D-M23251, ICD-10-D-M23259, ICD-10-D-M23222, ICD-10-D-M23221, ICD-10-D-M23229, ICD-10-D-M23201, ICD-10-D-M23200, ICD-10-D-M23202, ICD-10-D-M23204, ICD-10-D-M23203, ICD-10-D-M23205, ICD-10-D-M23207, ICD-10-D-M23206, ICD-10-D-M23209, ICD-10-D-S83282A, ICD-10-D-S83282S, ICD-10-D-S83282D, ICD-10-D-S83281A, ICD-10-D-S83281S, ICD-10-D-S83281D, ICD-10-D-S83289A, ICD-10-D-S83289S, ICD-10-D-S83289D, ICD-10-D-S83242A, ICD-10-D-S83242S, ICD-10-D-S83242D, ICD-10-D-S83241A, ICD-10-D-S83241S, ICD-10-D-S83241D, ICD-10-D-S83249A, ICD-10-D-S83249S, ICD-10-D-S83249D, ICD-10-D-S83204A, ICD-10-D-S83204S, ICD-10-D-S83204D, ICD-10-D-S83203A, ICD-10-D-S83203S, ICD-10-D-S83203D, ICD-10-D-S83205A, ICD-10-D-S83205S, ICD-10-D-S83205D, ICD-10-D-S83262A, ICD-10-D-S83262S, ICD-10-D-S83262D, ICD-10-D-S83261A, ICD-10-D-S83261S, ICD-10-D-S83261D, ICD-10-D-S83269A, ICD-10-D-S83269S, ICD-10-D-S83269D, ICD-10-D-S83222A, ICD-10-D-S83222S, ICD-10-D-S83222D, ICD-10-D-S83221A, ICD-10-D-S83221S, ICD-10-D-S83221D, ICD-10-D-S83229A, ICD-10-D-S83229S, ICD-10-D-S83229D, ICD-10-D-S83207A, ICD-10-D-S83207S, ICD-10-D-S83207D, ICD-10-D-S83206A, ICD-10-D-S83206S, ICD-10-D-S83206D, ICD-10-D-S83209A, ICD-10-D-S83209S, ICD-10-D-S83209D |
Cartilage injury | ICD-9-D-71800, ICD-9-D-71808, ICD-9-D-73390, ICD-9-D-73399, ICD-9-D-8360, ICD-9-D-8361, ICD-9-D-8362, ICD-10-D-S8330XA, ICD-10-D-S8330XD, ICD-10-D-S8330XS, ICD-10-D-S8331XA, ICD-10-D-S8331XD, ICD-10-D-S8331XS, ICD-10-D-S8332XA, ICD-10-D-S8332XD, ICD-10-D-S8332XS, ICD-10-D-M93261, ICD-10-D-M93262, ICD-10-D-M93269, ICD-9-D-7327, ICD-9-D-73392, ICD-9-D-7324, ICD-10-D-M9251, ICD-10-D-M9252, ICD-10-D-M9250, ICD-10-D-M9240, ICD-10-D-M9241, ICD-10-D-M9242, ICD-9-D-7177, ICD-10-D-M2240, ICD-10-D-M2241, ICD-10-D-M2242, ICD-10-D-M94261, ICD-10-D-M94262, ICD-10-D-M94269 |
Ligament injury | ICD-9-D-71781, ICD-9-D-71782, ICD-9-D-71783, ICD-9-D-71784, ICD-9-D-71785, ICD-10-D-M23601, ICD-10-D-M23602, ICD-10-D-M23609, ICD-10-D-M23611, ICD-10-D-M23612, ICD-10-D-M23619, ICD-10-D-M23621, ICD-10-D-M23622, ICD-10-D-M23629, ICD-10-D-M23631, ICD-10-D-M23632, ICD-10-D-M23639, ICD-10-D-M23641, ICD-10-D-M23642, ICD-10-D-M23649 |
Appendix B
Codes used to define complications and subsequent surgery
Complication | Codes |
|---|---|
Pulmonary embolism | ICD-9-D-4151:ICD-9-D-4159,ICD-10-D-I26:ICD-10-D-I269 |
Deep venous thrombosis | ICD-9-D-4532,ICD-9-D-4533,ICD-9-D-4534,ICD-9-D-45382,ICD-9-D-45384,ICD-9-D-45385,ICD-9-D 45386,ICD-10-D-I26:ICD-10-D-I2699 |
Pneumonia | ICD-9-D-4800:ICD-9-D-4809,ICD-9-D-481,ICD-9-D-4820,ICD-9-D-4821,ICD-9-D- 48230,ICD-9-D-48231,ICD-9-D-48232,ICD-9-D-48239,ICD-9-D-48240,ICD-9-D-48241,ICD-9-D-48242,ICD-9- D-48249,ICD-9-D-48281,ICD-9-D-48282,ICD-9-D-48283,ICD-9-D-48284,ICD-9-D-48289,ICD-9-D-4829,ICD-9- D-4830,ICD-9-D-4831,ICD-9-D-4838,ICD-9-D-4841,ICD-9-D-4843,ICD-9-D-4845,ICD-9-D-4846,ICD-9-D- 4847,ICD-9-D-4848,ICD-9-D-485,ICD-9-D-486,ICD-10-D-J12:ICD-10-D-J189 |
Acute kidney injury | ICD-9-D-5845,ICD-9-D-5846,ICD-9-D-5847,ICD-9-D-5848,ICD-9-D-5849,ICD-10D-N17:ICD-10-D-N179 |
Hematoma | ICD-9-D-99811,ICD-9-D-99812,ICD-9-D-99813,ICD-10-D-D7801, ICD-10-D-D7802, ICD-10-D-D7821, ICD-10-D-D7822, ICD-10-D-E3601, ICD-10-D-E3602, ICD-10-D-E89810, ICD-10-D-E89811, ICD-10-D-G9731, ICD-10-D-G9732, ICD-10-D-G9751, ICD-10-D-G9752, ICD-10-D-H59111, ICD-10-D- H59112, ICD-10-D-H59113, ICD-10-D-H59119, ICD-10-D-H59121, ICD-10-D-H59122, ICD-10-D-H59123, ICD-10-D-H59129, ICD-10-D-H59311, ICD-10-D-H59312, ICD-10-D-H59313, ICD-10-D-H59319, ICD-10-D- H59321, ICD-10-D-H59322, ICD-10-D-H59323, ICD-10-D-H59329, ICD-10-D-H9521, ICD-10-D-H9522, ICD-10-D-H9541, ICD-10-D-H9542, ICD-10-D-I97410, ICD-10-D-I97411, ICD-10-D-I97418, ICD-10-D-I9742, ICD-10-D-I97610, ICD-10-D-I97611, ICD-10-D-I97618, ICD-10-D-I97620, ICD-10-D-J9561, ICD-10-D-J9562, ICD- 10-D-J95830, ICD-10-D-J95831, ICD-10-D-K9161, ICD-10-D-K9162, ICD-10-D-K91840, ICD-10-D-K91841, ICD-10-D-L7601, ICD-10-D-L7602, ICD-10-D-L7621, ICD-10-D-L7622, ICD-10-D-M96810, ICD-10-D- M96811, ICD-10-D-M96830, ICD-10-D-M96831, ICD-10-D-N9961, ICD-10-D-N9962, ICD-10-D-N99820, ICD- 10-D-N99821, ICD-10-D-T888XXA |
Sepsis or septic shock | ICD-9-D-99591, ICD-9-D-99592, ICD-9-D-99802, ICD-9-D-99809, ICD-9-D-99800, ICD-10-D-A419, ICD-10-D-R6521, ICD-10-D-R6520, ICD-10-D-T8144XA, ICD-10-D-A400, ICD-10-D-A401, ICD-10-D-A4101, ICD-10-D-A4102, ICD-10-D-A411 |
Peroneal nerve injury | ICD-9-D-9563, ICD-10-D-S8410XA, ICD-10-D-S8411XA, ICD-10-D-S8412XA |
Popliteal artery injury | ICD-10-D-S85001A, ICD-10-D-85002A, ICD-10-D-85009A, ICD-9-D-9044, ICD-9-D-90441, ICD-9-D-90440, ICD-10-D-S85011A, ICD-10-D-S85012A, ICD-10-D-S85091A, ICD-10-D-S85092A |
Compartment syndrome | ICD-9-D-95890, ICD-9-D-72972, ICD-10-D-M79A21, ICD-10-D-M79A22, ICD-10-D-M79A29, ICD-10-D-T79A0XA |
Infection or drainage | ICD-9-D-71106, ICD-9-D-71146, ICD-9-D-71186, ICD-9-D-71196, ICD-9-D-99851, ICD-10-D-M01X61, ICD-10-D-M01X62, ICD-10-D-M01X69, CPT-10180, CPT-20005, CPT-27310, CPT-29871, ICD-9-D-99859, ICD-10-D-M00869, ICD-10-D-M00069, ICD-10-D-M00162, ICD-10-D-M00169, ICD-10-D-M00061, ICD-10-D-M00062, ICD-10-D-M00161, ICD-10-D-M00261, ICD-10-D-M00262, ICD-10-D-M00861, ICD-10-D-M00862, ICD-10-D-T847XXA, ICD-10-D-T84620A, ICD-10-D-T84621A, ICD-10-D-T84622A, ICD-10-D-T84623A, ICD-10-D-T84629A, ICD-9-D-99667 |
Wound disruption | ICD-9-D-99830,ICD-9-D-99831,ICD-9-D-99832,ICD-9-D-99833,ICD-10-D-T8130XA,ICD-10-D-T8130XD,ICD-10-D-T8130XS,ICD-10-D-T8131XA,ICD-10-D-T8131XD,ICD-10-D-T8131XS,ICD-10-D-T8132XA,ICD-10-D-T8132XD,ICD-10-D-T8132XS,ICD-10-D-T8133XA,ICD-10-D-T8133XD,ICD-10-D-T8133XS |
Any hardware-related complication | ICD-9-D-99640, ICD-9-D-99649, ICD-10-D-T84114A, ICD-10-D-T84115A, ICD-10-D-T84116A, ICD-10-D-T84117A, ICD-10-D-T84119A, ICD-10-D-T85698A, ICD-9-D-99678, ICD-10-D-T84124A, ICD-10-D-T84125A, ICD-10-D-T84126A, ICD-10-D-T84127A, ICD-10-D-T8481XA, ICD-10-D-T8486XA, ICD-10-D-T84418A, ICD-10-D-T84428A, ICD-10-D-T84498A, ICD-10-D-T847XXA, ICD-10-D-T84620A, ICD-10-D-T84621A, ICD-10-D-T84622A, ICD-10-D-T84623A, ICD-10-D-T84629A, ICD-9-D-99667 |
Hardware complications (mechanical or other) | ICD-9-D-99640, ICD-9-D-99649, ICD-10-D-T84114A, ICD-10-D-T84115A, ICD-10-D-T84116A, ICD-10-D-T84117A, ICD-10-D-T84119A, ICD-10-D-T85698A, ICD-9-D-99678, ICD-10-D-T84124A, ICD-10-D-T84125A, ICD-10-D-T84126A, ICD-10-D-T84127A, ICD-10-D-T8481XA, ICD-10-D-T8486XA, ICD-10-D-T84418A, ICD-10-D-T84428A, ICD-10-D-T84498A |
Hardware-related infection | ICD-10-D-T847XXA, ICD-10-D-T84620A, ICD-10-D-T84621A, ICD-10-D-T84622A, ICD-10-D-T84623A, ICD-10-D-T84629A, ICD-9-D-99667 |
Nonunion or malunion | ICD-9-D-73382, ICD-10-D-S8290XK, ICD-10-D-S72401K, ICD-10-D-S72402K, ICD-10-D-S72409K, ICD-10-D-S7290XK, ICD-10-D-S7291XK, ICD-10-D-S7292XK, ICD-10-D-S82101K, ICD-10-D-S82102K, ICD-9-D-73381, ICD-10-D-S72401P, ICD-10-D-S72402P, ICD-10-D-S72409P, ICD-10-D-S7290XP, ICD-10-D-S82101P, ICD-10-D-S82102P, ICD-10-D-S82109P |
Subsequent surgery | Codes |
|---|---|
Total knee arthroplasty | CPT-27445, CPT-27447, ICD-9-P-8154, ICD-10-P-0SRD0J9, ICD-10-P-0SRC0J9, ICD-10-P-0SRC0JA, ICD-10-P-0SRD0JA, ICD-10-P-0SRC069, ICD-10-P-0SRC06A, ICD-10-P-0SRC06Z, ICD-10-P-0SRC0JZ, ICD-10-P-0SRD069, ICD-10-P-0SRD06A, ICD-10-P-0SRD06Z, ICD-10-P-0SRD0JZ |
Unicompartmental knee arthroplasty | CPT-27446, ICD-10-P-0SRC0L9, ICD-10-P-0SRC0LA, ICD-10-P-0SRC0LZ, ICD-10-P-0SRD0L9, ICD-10-P-0SRD0LA, ICD-10-P-0SRD0LZ, ICD-10-P-0SRC0M9, ICD-10-P-0SRC0MA, ICD-10-P-0SRC0MZ, ICD-10-P-0SRD0M9, ICD-10-P-0SRD0MA, ICD-10-P-0SRD0MZ |
Manipulation under anesthesia | CPT-27570 |
Any arthroscopic procedure | CPT-29884, ICD-9-P-8026, ICD-10-P-0SJC4ZZ, ICD-10-P-0SJD4ZZ, CPT-29866, CPT-29867, CPT-29874, CPT-29877, CPT-29879, CPT-29885, CPT-29886, CPT-29887, CPT-G0289 |
Arthroscopy with cartilage procedure | CPT-29866, CPT-29867, CPT-29874, CPT-29877, CPT-29879, CPT-29885, CPT-29886, CPT-29887, CPT-G0289 |
Hardware removal | CPT-20680, ICD-9-P-7865, ICD-9-P-7867, ICD-10-P-0QPB04Z, ICD-10-P-0QPB34Z, ICD-10-P-0QPB44Z, ICD-10-P-0QPC04Z, ICD-10-P-0QPC34Z, ICD-10-P-0QPC44Z, ICD-10-P-0QPG04Z, ICD-10-P-0QPG34Z, ICD-10-P-0QPG44Z, ICD-10-P-0QPH04Z, ICD-10-P-0QPH34Z, ICD-10-P-0QPH44Z |
Co-morbidity | Codes |
|---|---|
Diabetes mellitus | ICD-9-D-24900:ICD-9-D-25099,ICD-9-D-7902,ICD-9-D-79021,ICD-9-D-79022,ICD-9-D-79029,ICD-9-D-7915,ICD-9-D-7916,ICD-10-D-E090:ICD-10-D-E139 |
Tobacco use | ICD-9-D-3051, ICD-9-D-V1582, ICD-10-D-F17220, ICD-10-D-F17221, ICD-10-D-F17223, ICD-10-D-F17228, ICD-10-D-F17229, ICD-10-D-F17290, ICD-10-D-F17291, ICD-10-D-F17293, ICD-10-D-F17298, ICD-10-D-F17299, ICD-10-D-Z720 |
Obesity | ICD-9-D-2780,ICD-9-D-27800,ICD-9-D-27801,ICD-9-D-27802,ICD-9-D-27803,ICD-10-D-E660:ICD-10-D-E669 |
Appendix C
Variables included in multiple logistic regression.
HTO 90-day complications
Complication | Variables included |
|---|---|
Wound disruption | Obesity, ECI, diabetes |
Infection | Obesity, gender, ECI |
Readmission | ECI, obesity, diabetes |
All hardware-related complications | ECI, age, diabetes, tobacco |
Mechanical or “other” hardware complications | Tobacco, ECI, gender |
Hardware-related infections | ECI, obesity, diabetes |
DFO 90-day complications
Complication | Variables included |
|---|---|
Wound disruption | None, n < 20 per group |
Infection | ECI, obesity, diabetes |
Readmission | ECI, age > 40 |
All hardware-related complications | ECI, age > 40 |
Mechanical or “other” hardware complications | None, n < 20 per group |
Hardware-related infections | None, n < 20 per group |
HTO 2-year complication
Complication | Variables included |
|---|---|
Wound disruption | Obesity, diabetes, ECI, age |
Infection | Obesity, diabetes, ECI, age |
All hardware-related complications | Gender, ECI, age, tobacco |
Mechanical or “other” hardware complications | Age, gender, tobacco |
Hardware-related infections | Obesity, diabetes, ECI |
Nonunion or malunion | Obesity, ECI, tobacco |
DFO 2 year complication
Complication | Variables included |
|---|---|
Wound disruption | None, n < 20 per group |
Infection | ECI, obesity, diabetes |
All hardware-related complications | None, no factors identified in univariate analysis |
Mechanical or “other” hardware complications | None, no factors identified in univariate analysis |
Hardware-related infections | ECI, age > 40 |
Nonunion or malunion | None, no factors identified in univariate analysis |
DFO re-operation
Operation | Variables included |
|---|---|
TKA | ECI, age |
MUA | None, no factors identified in univariate analysis |
Any arthroscopic procedure | Age < 40, gender |
Arthroscopy with cartilage procedure | Age < 40, gender |
Hardware removal | Age < 40, gender, obesity |
HTO re-operation
Operation | Variables included |
|---|---|
TKA | Diabetes, ECI, age > 40 |
MUA | Age, gender |
Any arthroscopic procedure | Age < 40, gender |
Arthroscopy with cartilage procedure | Age, gender |
Hardware removal | Age < 40, gender, obesity |
Rights and permissions
About this article
Cite this article
Kucirek, N.K., Anigwe, C., Zhang, A.L. et al. Complications after high tibial osteotomy and distal femoral osteotomy are associated with increasing medical comorbidities and tobacco use. Knee Surg Sports Traumatol Arthrosc 30, 4029–4045 (2022). https://doi.org/10.1007/s00167-022-06865-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-06865-z