Abstract
Purpose
To evaluate the effect of posterior tibial slope (PTS) on patient-reported outcomes (PROs) and posterior cruciate ligament (PCL) graft failure after PCL reconstruction.
Methods
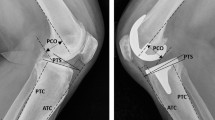
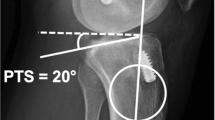
Patients undergoing PCL reconstruction with a minimum 2-year follow-up were included in this retrospective cohort study. A chart review was performed to collect patient-, injury-, and surgery-related data. Medial PTS was measured on preoperative lateral radiographs. Validated PROs, including the International Knee Documentation Committee Subjective Knee Form, Knee injury and Osteoarthritis Outcome Score, Lysholm Score, Tegner Activity Scale, and Visual Analogue Scale for pain, were collected at final follow-up. A correlation analysis was conducted to assess the relationship between PTS and PROs. A logistic regression model was performed to evaluate if PTS could predict PCL graft failure.
Results
Overall, 79 patients with a mean age of 28.6 ± 11.7 years and a mean follow-up of 5.7 ± 3.3 years were included. After a median time from injury of 4.0 months, isolated and combined PCL reconstruction was performed in 22 (28%) and 57 (72%) patients, respectively. There were no statistically significant differences in PROs and PTS between patients undergoing isolated and combined PCL reconstruction (non-significant [n.s.]). There were no significant correlations between PTS and PROs (n.s.). In total, 14 (18%) patients experienced PCL graft failure after a median time of 17.5 months following PCL reconstruction. Patients with PCL graft failure were found to have statistically significantly lower PTS than patients without graft failure (7.0 ± 2.3° vs. 9.2 ± 3.3°, p < 0.05), while no differences were found in PROs (n.s.). PTS was shown to be a significant predictor of PCL graft failure, with a 1.3-fold increase in the odds of graft failure for each one-degree reduction in PTS (p < 0.05).
Conclusions
This study showed that PTS does not affect PROs after PCL reconstruction, but that PTS represents a surgically modifiable predictor of PCL graft failure.
Level of evidence
III.


Similar content being viewed by others
References
Winkler PW, Zsidai B, Wagala NN, Hughes JD, Horvath A, Senorski EH et al (2020) Evolving evidence in the treatment of primary and recurrent posterior cruciate ligament injuries, part 1: anatomy, biomechanics and diagnostics. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06357-y
Winkler PW, Zsidai B, Wagala NN, Hughes JD, Horvath A, Senorski EH et al (2020) Evolving evidence in the treatment of primary and recurrent posterior cruciate ligament injuries, part 2: surgical techniques, outcomes and rehabilitation. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06337-2
Lee DW, Kim JG, Yang SJ, Cho SI (2019) Return to sports and clinical outcomes after arthroscopic anatomic posterior cruciate ligament reconstruction with remnant preservation. Arthroscopy 35:2658-2668.e2651
Lutz PM, Merkle M, Winkler PW, Geyer S, Herbst E, Braun S et al (2021) Combined posterolateral knee reconstruction: ACL-based injuries perform better compared to PCL-based injuries. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06409-3
Tucker CJ, Cotter EJ, Waterman BR, Kilcoyne KG, Cameron KL, Owens BD (2019) Functional outcomes after isolated and combined posterior cruciate ligament reconstruction in a military population. Orthop J Sports Med 7:2325967119875139
Noyes FR, Barber-Westin SD (2005) Posterior cruciate ligament revision reconstruction, part 1: causes of surgical failure in 52 consecutive operations. Am J Sports Med 33:646–654
Bernhardson AS, Aman ZS, DePhillipo NN, Dornan GJ, Storaci HW, Brady AW et al (2019) Tibial slope and its effect on graft force in posterior cruciate ligament reconstructions. Am J Sports Med 47:1168–1174
Lee SH, Jung YB, Lee HJ, Jung HJ, Kim SH (2012) Revision posterior cruciate ligament reconstruction using a modified tibial-inlay double-bundle technique. J Bone Joint Surg Am 94:516–522
Bernhardson AS, DePhillipo NN, Daney BT, Kennedy MI, Aman ZS, LaPrade RF (2019) Posterior tibial slope and risk of posterior cruciate ligament injury. Am J Sports Med 47:312–317
Gwinner C, Weiler A, Roider M, Schaefer FM, Jung TM (2017) Tibial slope strongly influences knee stability after posterior cruciate ligament reconstruction: a prospective 5- to 15-year follow-up. Am J Sports Med 45:355–361
Winkler PW, Godshaw BM, Karlsson J, Getgood AMJ, Musahl V (2021) Posterior tibial slope: the fingerprint of the tibial bone. Knee Surg Sports Traumatol Arthrosc 29:1687–1689
Bernhardson AS, DePhillipo NN, Aman ZS, Kennedy MI, Dornan GJ, LaPrade RF (2019) Decreased posterior tibial slope does not affect postoperative posterior knee laxity after double-bundle posterior cruciate ligament reconstruction. Am J Sports Med 47:318–323
Schlumberger M, Schuster P, Eichinger M, Mayer P, Mayr R, Immendörfer M et al (2020) Posterior cruciate ligament lesions are mainly present as combined lesions even in sports injuries. Knee Surg Sports Traumatol Arthrosc 28:2091–2098
Schulz MS, Russe K, Weiler A, Eichhorn HJ, Strobel MJ (2003) Epidemiology of posterior cruciate ligament injuries. Arch Orthop Trauma Surg 123:186–191
Pfeiffer TR, Burnham JM, Hughes JD, Kanakamedala AC, Herbst E, Popchak A et al (2018) An increased lateral femoral condyle ratio is a risk factor for anterior cruciate ligament injury. J Bone Joint Surg Am 100:857–864
Weinberg DS, Williamson DF, Gebhart JJ, Knapik DM, Voos JE (2017) Differences in medial and lateral posterior tibial slope: an osteological review of 1090 tibiae comparing age, sex, and race. Am J Sports Med 45:106–113
Napier RJ, Garcia E, Devitt BM, Feller JA, Webster KE (2019) Increased radiographic posterior tibial slope is associated with subsequent injury following revision anterior cruciate ligament reconstruction. Orthop J Sports Med 7:2325967119879373
Winkler PW, Wagala NN, Hughes JD, Lesniak BP, Musahl V (2021) A high tibial slope, allograft use, and poor patient-reported outcome scores are associated with multiple ACL graft failures. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06460-8
Lind M, Nielsen TG, Behrndtz K (2018) Both isolated and multi-ligament posterior cruciate ligament reconstruction results in improved subjective outcome: results from the Danish knee ligament reconstruction registry. Knee Surg Sports Traumatol Arthrosc 26:1190–1196
Harner CD, Janaushek MA, Kanamori A, Yagi M, Vogrin TM, Woo SL (2000) Biomechanical analysis of a double-bundle posterior cruciate ligament reconstruction. Am J Sports Med 28:144–151
Harner CD, Janaushek MA, Ma CB, Kanamori A, Vogrin TM, Woo SL (2000) The effect of knee flexion angle and application of an anterior tibial load at the time of graft fixation on the biomechanics of a posterior cruciate ligament-reconstructed knee. Am J Sports Med 28:460–465
Harner CD, Vogrin TM, Höher J, Ma CB, Woo SL (2000) Biomechanical analysis of a posterior cruciate ligament reconstruction. Deficiency of the posterolateral structures as a cause of graft failure. Am J Sports Med 28:32–39
Lee DY, Kim DH, Kim HJ, Ahn HS, Lee TH, Hwang SC (2018) Posterior cruciate ligament reconstruction with transtibial or tibial inlay techniques: a meta-analysis of biomechanical and clinical outcomes. Am J Sports Med 46:2789–2797
Akoto R, Alm L, Drenck TC, Frings J, Krause M, Frosch KH (2020) Slope-correction osteotomy with lateral extra-articular tenodesis and revision anterior cruciate ligament reconstruction is highly effective in treating high-grade anterior knee laxity. Am J Sports Med 48:3478–3485
Song GY, Ni QK, Zheng T, Zhang ZJ, Feng H, Zhang H (2020) Slope-reducing tibial osteotomy combined with primary anterior cruciate ligament reconstruction produces improved knee stability in patients with steep posterior tibial slope, excessive anterior tibial subluxation in extension, and chronic meniscal posterior horn tears. Am J Sports Med 48:3486–3494
Giffin JR, Stabile KJ, Zantop T, Vogrin TM, Woo SL, Harner CD (2007) Importance of tibial slope for stability of the posterior cruciate ligament deficient knee. Am J Sports Med 35:1443–1449
Yoon KH, Park SY, Park JY, Kim EJ, Kim SJ, Kwon YB et al (2020) Influence of posterior tibial slope on clinical outcomes and survivorship after anterior cruciate ligament reconstruction using hamstring autografts: a minimum of 10-year follow-up. Arthroscopy 36:2718–2727
Bernhardson AS, Aman ZS, Dornan GJ, Kemler BR, Storaci HW, Brady AW et al (2019) Tibial slope and its effect on force in anterior cruciate ligament grafts: anterior cruciate ligament force increases linearly as posterior tibial slope increases. Am J Sports Med 47:296–302
Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD (2004) Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med 32:376–382
Funding
No funding was received for the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All listed authors have contributed substantially to this work: PWW, NNW, MF, EMN, SC, and JDH collected data, and performed statistical analysis, literature review, and primary manuscript preparation. VM, BPL, DV, SR, and JJI assisted with interpretation of the results as well as editing and final manuscript preparation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
VM reports educational grants, consulting fees, and speaking fees from Smith & Nephew plc, educational grants from Arthrex, is a board member of the International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine (ISAKOS), and Deputy Editor-in-Chief of Knee Surgery, Sports Traumatology, Arthroscopy (KSSTA). DV reports consulting fees from Arthrex and is a member of the editorial board of The American Journal of Sports Medicine.
Ethical approval
This study was approved by the Institutional Review Board of the University of Pittsburgh (No.: STUDY20070271).
Informed consent
Written informed consent was obtained from each patient who completed the questionnaire of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The investigation was performed at the Department of Orthopaedic Surgery, University of Pittsburgh, Pittsburgh, PA, USA.
Rights and permissions
About this article
Cite this article
Winkler, P.W., Wagala, N.N., Carrozzi, S. et al. Low posterior tibial slope is associated with increased risk of PCL graft failure. Knee Surg Sports Traumatol Arthrosc 30, 3277–3286 (2022). https://doi.org/10.1007/s00167-021-06760-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-021-06760-z