Abstract
Purpose
The priorities of patients should be shared by those treating them. Patients and surgeons are likely to have different priorities surrounding anterior cruciate ligament reconstruction (ACLR), with implications for shared decision-making and patient education. The optimal surgical approach for ACLR is constantly evolving, and the magnitude of treatment effect necessary for evidence to change surgical practice is unknown. The aim of this study was to determine (1) the priorities of surgeons and patients when making decisions regarding ACLR and (2) the magnitude of reduction in ACLR graft failure risk that orthopaedic surgeons require before changing practice.
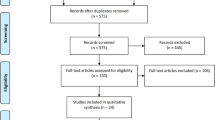
Methods
This study followed a cross-sectional survey design. Three distinct electronic surveys were administered to pre-operative ACLR patients, post-operative ACLR patients, and orthopaedic surgeons. Patients and surgeons were asked about the importance of various outcomes and considerations pertaining to ACLR. Surgeons were asked scenario-based questions regarding changing practice for ACLR based on new research.
Results
Surgeons were more likely to prioritize outcomes related to the surgical knee itself, whereas patients were more likely to prioritize outcomes related to their daily lifestyle and activities. Knee instability and risk of re-injury were unanimous top priorities among all three groups. A mean relative risk reduction in ACLR graft failure of about 50% was required by orthopaedic surgeons to change practice regardless of the type of change, or patient risk profile.
Conclusion
There are discrepancies between the priorities of surgeons and patients, and orthopaedic surgeons appear resistant to changing practice for ACLR.
Level of evidence
IV.


Similar content being viewed by others
Abbreviations
- ACL:
-
Anterior cruciate ligament
- ACLR:
-
Anterior cruciate ligament reconstruction
- ACLSG:
-
ACL Study Group
- RD:
-
Risk difference
- RRR:
-
Relative risk reduction
- CI:
-
Confidence interval
- RCTs:
-
Randomized clinical trials
- OA:
-
Osteoarthritis
References
Adie S, Harris IA, Naylor JM, Mittal R (2017) Are outcomes reported in surgical randomized trials patient-important? A systematic review and meta-analysis. Can J Surg 60:86–93
Bhandari M, Montori V, Devereaux PJ, Dosanjh S, Sprague S, Guyatt GH (2003) Challenges to the practice of evidence-based medicine during residents’ surgical training: a qualitative study using grounded theory. Acad Med 78:1183–1190
Carey JL, Shea KG (2015) AAOS clinical practice guideline: management of anterior cruciate ligament injuries: evidence-based guideline. J Am Acad Orthop Surg 23:e6–e8
Cheung SC, Allen CR, Gallo RA, Ma CB, Feeley BT (2012) Patients’ attitudes and factors in their selection of grafts for anterior cruciate ligament reconstruction. Knee 19:49–54
Cohen SB, Yucha DT, Ciccotti MC, Goldstein DT, Ciccotti MA, Ciccotti MG (2009) Factors affecting patient selection of graft type in anterior cruciate ligament reconstruction. Arthroscopy 25:1006–1010
Cole BJ, Cotter EJ, Wang KC, Davey A (2017) Patient understanding, expectations, outcomes, and satisfaction regarding anterior cruciate ligament injuries and surgical management. Arthroscopy 33:1092–1096
Dillman DA, Smyth JD, Christian LM (2014) Ordering questions and testing for question order effects. In: Internet, phone, mail, and mixed-mode surveys: the tailored design method. Wiley, pp 228–257
Dyson MP, Shave K, Gates A, Fernandes RM, Scott SD, Hartling L (2017) Which outcomes are important to patients and families who have experienced paediatric acute respiratory illness? Findings from a mixed methods sequential exploratory study. BMJ Open 7:1–10
Feucht MJ, Cotic M, Saier T, Minzlaff P, Plath JE, Imhoff AB, Hinterwimmer S (2016) Patient expectations of primary and revision anterior cruciate ligament reconstruction. Knee Surg Sport Traumatol Arthrosc 24:201–207
Getgood AMJ, Bryant DM, Litchfield R, Heard M, McCormack RG, Rezansoff A, Peterson D, Bardana D, MacDonald PB, Verdonk PCM, Spalding T, Willits K, Birmingham T, Hewison C, Wanlin S, Firth A, Pinto R, Martindale A, O’Neill L, Jennings M, Daniluk M, Boyer D, Zomar M, Moon K, Pritchett R, Payne K, Fan B, Mohan B, Buchko GM, Hiemstra LA, Kerslake S, Tynedal J, Stranges G, Mcrae S, Gullett LA, Brown H, Legary A, Longo A, Christian M, Ferguson C, Mohtadi N, Barber R, Chan D, Campbell C, Garven A, Pulsifer K, Mayer M, Simunovic N, Duong A, Robinson D, Levy D, Skelly M, Shanmugaraj A, Howells F, Tough M, Spalding T, Thompson P, Metcalfe A, Asplin L, Dube A, Clarkson L, Brown J, Bolsover A, Bradshaw C, Belgrove L, Millan F, Turner S, Verdugo S, Lowe J, Dunne D, McGowan K, Suddens CM, Declercq G, Vuylsteke K, Van Haver M (2020) Lateral extra-articular tenodesis reduces failure of hamstring tendon autograft anterior cruciate ligament reconstruction: 2-year outcomes from the STABILITY study randomized clinical trial. Am J Sports Med 48:285–297
Guyatt G, Haynes B, Jaeschke R, Meade MO, Wilson M, Montori V, Richardson S (2008) The philosophy of evidence based medicine. In: Users’ guide to the medical literature. McGraw-Hill Medical, pp 1–14
Kamath GV, Redfern JC, Greis PE, Burks RT (2011) Revision anterior cruciate ligament reconstruction. Am J Sports Med 39:199–217
Lohmander SL, Englund MP, Dahl LL, Roos EM (2007) The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med 35:1756–1769
Mather RC, Koenig L, Kocher MS, Dall TM, Gallo P, Scott DJ, Bach BR, Spindler KP (2013) Societal and economic impact of anterior cruciate ligament tears. J Bone Jt Surg 95:1751–1759
Mohtadi NG, Chan DS (2019) A randomized clinical trial comparing patellar tendon, hamstring tendon, and double-bundle ACL reconstructions: patient-reported and clinical outcomes at 5-year follow-up. J Bone Jt Surg 101:949–960
Nwachukwu BU, Adjei J, Rauck RC, Chahla J, Okoroha KR, Verma NN, Allen AA, Williams RJ (2019) How much do psychological factors affect lack of return to play after anterior cruciate ligament reconstruction? A systematic review. Orthop J Sport Med 7:1–7
Sanders TL, Maradit Kremers H, Bryan AJ, Larson DR, Dahm DL, Levy BA, Stuart MJ, Krych AJ (2016) Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med 44:1502–1507
Schober P, Schwarte LA (2018) Correlation coefficients: appropriate use and interpretation. Anesth Analg 126:1763–1768
Spindler KP, Huston LJ, Zajichek A, Reinke EK, Amendola A, Andrish JT, Brophy RH, Dunn WR, Flanigan DC, Jones MH, Kaeding CC, Marx RG, Matava MJ, McCarty EC, Parker RD, Vidal AF, Wolcott ML, Wolf BR, Wright RW (2020) Anterior cruciate ligament reconstruction in high school and college-aged athletes: does autograft choice influence anterior cruciate ligament revision rates? Am J Sports Med 48:298–309
Thornley P, De Sa D, Evaniew N, Farrokhyar F, Bhandari M, Ghert M (2016) An international survey to identify the intrinsic and extrinsic factors of research studies most likely to change orthopaedic practice. Bone Jt Res 5:130–136
Webster KE, Feller JA, Leigh WB, Richmond AK (2014) Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med 42:641–647
Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD (2016) Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction. Am J Sports Med 44:1861–1876
Wright RW, Huston LJ, Haas AK, Allen CR, Anderson AF, Cooper DE, DeBerardino TM, Dunn WR, Lantz BA, Mann B, Spindler KP, Stuart MJ, Nwosu SK, Pennings JS, Albright JP, Amendola A, Andrish JT, Annunziata CC, Arciero RA, Bach BR, Baker CL, Bartolozzi AR, Baumgarten KM, Bechler JR, Berg JH, Bernas GA, Brockmeier SF, Brophy RH, Bush-Joseph CA, Butler JB, Campbell JD, Carey JL, Carpenter JE, Cole BJ, Cooper JM, Cox CL, Creighton RA, Dahm DL, David TS, Flanigan DC, Frederick RW, Ganley TJ, Garofoli EA, Gatt CJ, Gecha SR, Giffin JR, Hame SL, Hannafin JA, Harner CD, Harris NL, Hechtman KS, Hershman EB, Hoellrich RG, Hosea TM, Johnson DC, Johnson TS, Jones MH, Kaeding CC, Kamath GV, Klootwyk TE, Levy BA, Ma CB, Maiers GP, Marx RG, Matava MJ, Mathien GM, McAllister DR, McCarty EC, McCormack RG, Miller BS, Nissen CW, O’Neill DF, Owens BD, Parker RD, Purnell ML, Ramappa AJ, Rauh MA, Rettig AC, Sekiya JK, Shea KG, Sherman OH, Slauterbeck JR, Smith MV, Spang JT, Svoboda LSJ, Taft TN, Tenuta JJ, Tingstad EM, Vidal AF, Viskontas DG, White RA, Williams JS, Wolcott ML, Wolf BR, York JJ (2020) Predictors of clinical outcome following revision anterior cruciate ligament reconstruction. J Orthop Res 38:1191–1203
Acknowledgements
The authors would like to thank the ACL Study Group for participating in this study. The authors would also like to acknowledge Dr. Robert Litchfield, Dr. Kevin Willits and Dr. Ryan Degen for allowing their patients to be recruited for this study.
Funding
No funding was provided for this study.
Author information
Authors and Affiliations
Contributions
HM helped with study conception and design, completed data collection, completed statistical analysis, helped with interpretation of the data and drafted the manuscript. DMB helped with study conception and design, statistical analysis, interpretation of the data and drafting the manuscript. TBB helped with study conception and design, interpretation of the data and drafting the manuscript. AK helped with study conception and design, interpretation of the data and drafting the manuscript. KPS helped with interpretation of the data and critically revised the manuscript. CCK helped with data collection, interpretation of the data and critically revised the manuscript. TS helped with data collection, interpretation of the data and critically revised the manuscript. AMJG helped with study conception and design, data collection, interpretation of the data and drafting the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
H.M., D.M.B, T.B.B. and K.T. declare that they have no competing interests. K.P.S. has received consulting fees from the National Football League, Service Excellence, Mitek, Flexion, Samumed and Novopeds; research funding from Smith & Nephew Endoscopy, DonJoy Orthopedics and NIH/NIAMS; and hospitality payments from DePuy and Biosense Webster. C.C.K. was the past president of the ACL Study Group and has received research funding from DJO and Zimmer Biomet, consulting fees from Zimmer Biomet, education payments from CDC Medical, and compensation for services other than consulting from Arthrex. T.S. is the President of the ACL Study Group and has received speaking fees from Conmed, Smith & Nephew, and JRF Ortho, and royalties from Conmed. A.M.J.G. is the Program Chair of the ACL Study Group and has received royalties from Smith & Nephew and Graymont Inc, research funding from Smith & Nephew and Ossur, and consulting fees from Smith & Nephew, Ossur, and Olympus.
Ethical approval
This study was grant ethics approval by the Western University Health Science Research Ethics Board (Ref #: 114977).
Informed consent
Informed consent was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Marmura, H., Bryant, D.M., Birmingham, T.B. et al. Same knee, different goals: patients and surgeons have different priorities related to ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 29, 4286–4295 (2021). https://doi.org/10.1007/s00167-021-06550-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-021-06550-7