Abstract
Purpose
Recovery following elective knee arthroscopy can be compromised by prolonged postoperative opioid utilization, yet an effective and validated risk calculator for this outcome remains elusive. The purpose of this study is to develop and validate a machine-learning algorithm that can reliably and effectively predict prolonged opioid consumption in patients following elective knee arthroscopy.
Methods
A retrospective review of an institutional outcome database was performed at a tertiary academic medical centre to identify adult patients who underwent knee arthroscopy between 2016 and 2018. Extended postoperative opioid consumption was defined as opioid consumption at least 150 days following surgery. Five machine-learning algorithms were assessed for the ability to predict this outcome. Performances of the algorithms were assessed through discrimination, calibration, and decision curve analysis.
Results
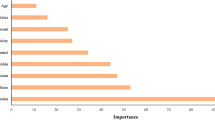
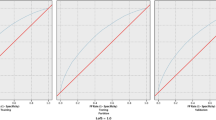
Overall, of the 381 patients included, 60 (20.3%) demonstrated sustained postoperative opioid consumption. The factors determined for prediction of prolonged postoperative opioid prescriptions were reduced preoperative scores on the following patient-reported outcomes: the IKDC, KOOS ADL, VR12 MCS, KOOS pain, and KOOS Sport and Activities. The ensemble model achieved the best performance based on discrimination (AUC = 0.74), calibration, and decision curve analysis. This model was integrated into a web-based open-access application able to provide both predictions and explanations.
Conclusion
Following appropriate external validation, the algorithm developed presently could augment timely identification of patients who are at risk of extended opioid use. Reduced scores on preoperative patient-reported outcomes, symptom duration and perioperative oral morphine equivalents were identified as novel predictors of prolonged postoperative opioid use. The predictive model can be easily deployed in the clinical setting to identify at risk patients thus allowing providers to optimize modifiable risk factors and appropriately counsel patients preoperatively.
Level of evidence
III.




Similar content being viewed by others
References
Frieden TR, Houry D (2016) Reducing the risks of relief-the CDC opioid-prescribing guideline. N Engl J Med 374:1501–1504
Stoicea N, Costa A, Periel L, Uribe A, Weaver T, Bergese SD (2019) Current perspectives on the opioid crisis in the US healthcare system: a comprehensive literature review. Medicine (Baltimore) 98:e15425
Dowell D, Haegerich TM, Chou R (2016) CDC guideline for prescribing opioids for chronic pain-United States, 2016. JAMA 315:1624–1645
Guy GP Jr, Zhang K, Bohm MK, Losby J, Lewis B, Young R et al (2017) Vital signs: changes in opioid prescribing in the United States, 2006–2015. MMWR Morb Mortal Wkly Rep 66:697–704
Gostin LO, Hodge JG Jr, Noe SA (2017) Reframing the opioid epidemic as a national emergency. JAMA 318:1539–1540
Reider B (2019) Opioid epidemic. Am J Sports Med 47:1039–1042
Brummett CM, Waljee JF, Goesling J, Moser S, Lin P, Englesbe MJ et al (2017) New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg 152:e170504
Jildeh TR, Taylor KA, Khalil LS, Okoroha KR, Matar RN, Geisenhoff A et al (2019) Risk factors for postoperative opioid use in arthroscopic meniscal surgery. Arthroscopy 35:575–580
Rao AG, Chan PH, Prentice HA, Paxton EW, Funahashi TT, Maletis GB (2019) Risk factors for opioid use after anterior cruciate ligament reconstruction. Am J Sports Med 47:2130–2137
Berglund DD, Rosas S, Kurowicki J, Horn B, Mijic D, Levy JC (2018) Preoperative opioid use among patients undergoing shoulder arthroplasty predicts prolonged postoperative opioid use. J Am Acad Orthop Surg 27:e691–e695
Khazi ZM, Lu Y, Patel BH, Cancienne JM, Werner B, Forsythe B (2020b) Risk factors for opioid use after total shoulder arthroplasty. J Shoulder Elbow Surg 29:235–243
Nicholson AD, Kassam HF, Steele JL, Passarelli NR, Blaine TA, Kovacevic D (2019) Development of a clinical risk calculator for prolonged opioid use after shoulder surgery. J Shoulder Elbow Surg 28:2225–2231
Gowd AK, Agarwalla A, Amin NH, Romeo AA, Nicholson GP, Verma NN et al (2019) Construct validation of machine learning in the prediction of short-term postoperative complications following total shoulder arthroplasty. J Shoulder Elbow Surg 28:e410–e421
Karhade AV, Ogink PT, Thio Q, Broekman MLD, Cha TD, Hershman SH et al (2019) Machine learning for prediction of sustained opioid prescription after anterior cervical discectomy and fusion. Spine J 19:976–983
Rahman SA, Walker RC, Lloyd MA, Grace BL, van Boxel GI, Kingma BF et al (2020) Machine learning to predict early recurrence after oesophageal cancer surgery. Br J Surg 107:1042–1052
Harris AHS, Kuo AC, Weng Y, Trickey AW, Bowe T, Giori NJ (2019) Can machine learning methods produce accurate and easy-to-use prediction models of 30-day complications and mortality after knee or hip arthroplasty? Clin Orthop Relat Res 477:452–460
Kim JS, Merrill RK, Arvind V, Kaji D, Pasik SD, Nwachukwu CC et al (2018) Examining the ability of artificial neural networks machine learning models to accurately predict complications following posterior lumbar spine fusion. Spine (Phila Pa 1976) 43:853–860
Collins GS, Reitsma JB, Altman DG, Moons KG (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. Br J Surg 102:148–158
Luo W, Phung D, Tran T, Gupta S, Rana S, Karmakar C et al (2016) Guidelines for developing and reporting machine learning predictive models in biomedical research: a multidisciplinary view. J Med Internet Res 18:e323
Hughes JD, Hughes JL, Bartley JH, Hamilton WP, Brennan KL (2017) Infection rates in arthroscopic versus open rotator cuff repair. Orthop J Sports Med 5:2325967117715416
Stekhoven DJ, Bühlmann P (2012) MissForest–non-parametric missing value imputation for mixed-type data. Bioinformatics 28:112–118
Dietterich TG (2000) Ensemble methods in machine learning. Berlin, Heidelberg
Steyerberg EW, Moons KG, van der Windt DA, Hayden JA, Perel P, Schroter S et al (2013) Prognosis research strategy (PROGRESS) 3: prognostic model research. PLoS Med 10:1
Raudys SJ, Jain AK (1991) Small sample size effects in statistical pattern recognition: recommendations for practitioners. IEEE Trans Pattern Anal Mach Intell 13:252–264
Gil JA, Gunaseelan V, DeFroda SF, Brummett CM, Bedi A, Waljee JF (2019) Risk of prolonged opioid use among opioid-naïve patients after common shoulder arthroscopy procedures. Am J Sports Med 47:1043–1050
Lu Y, Beletsky A, Cohn MR, Patel BH, Cancienne J, Nemsick M et al (2020) Perioperative opioid use predicts postoperative opioid use and inferior outcomes after shoulder arthroscopy. Arthroscopy. https://doi.org/10.1016/j.arthro.2020.05.044
Pullen SD, Acker C, Kim H, Mullins M, Sims P, Strasbaugh H et al (2020) Physical therapy for chronic pain mitigation and opioid use reduction among people living with human immunodeficiency virus in Atlanta. A Descriptive Case Series. AIDS Res Hum Retroviruses, GA
Rosa HZ, Barcelos RCS, Segat HJ, Roversi K, Dias VT, Milanesi LH et al (2020) Physical exercise modifies behavioral and molecular parameters related to opioid addiction regardless of training time. Eur Neuropsychopharmacol 32:25–35
Timm KE (1994) A randomized-control study of active and passive treatments for chronic low back pain following L5 laminectomy. J Orthop Sports Phys Ther 20:276–286
Jerant A, Agnoli A, Franks P (2020) Poorer physical and mental health status are associated with subsequent opioid prescriptions: a U.S. Natl Study J Gen Intern Med 35:554–560
Khazi ZM, Baron J, Shamrock A, Gulbrandsen T, Bedard N, Wolf B et al (2020a) Preoperative Opioid Usage, Male Gender, and Preexisting Knee OA Impacts Opioid Refills after Isolated Arthroscopic Meniscectomy: A Population Based Study. Arthroscopy. https://doi.org/10.1016/j.arthro.2020.04.039
Khazi ZM, Lu Y, Shamrock AG, Duchman KR, Westermann RW, Wolf BR (2019) Opioid use following shoulder stabilization surgery: risk factors for prolonged use. J Shoulder Elbow Surg 28:1928–1935
Han SB, Seo IW, Shin YS (2020) Intra-articular injections of hyaluronic acid or steroid associated with better outcomes than platelet-rich plasma, adipose mesenchymal stromal cell, or placebo in knee osteoarthritis: a network meta-analysis. Arthroscopy. https://doi.org/10.1016/j.arthro.2020.03.041
Wilson LA, Liu J, Fiasconaro M, Poeran J, Nwachukwu BU, Memtsoudis SG (2020) Increased use of intra-articular steroid injection to treat osteoarthritis is associated with chronic opioid dependence after later total knee arthroplasty but not total hip arthroplasty. J Arthroplasty. https://doi.org/10.1016/j.arth.2020.04.012
Wang D, Chang B, Coxe FR, Pais MD, Wickiewicz TL, Warren RF et al (2019) Clinically meaningful improvement after treatment of cartilage defects of the knee with osteochondral grafts. Am J Sports Med 47:71–81
Agarwalla A, Gowd AK, Liu JN, Lalehzarian SP, Christian DR, Cole BJ et al (2019) Predictive factors and duration to return to sport after isolated meniscectomy. Orthop J Sports Med 7:2325967119837940
Edwards PK, Ebert JR, Joss B, Ackland T, Annear P, Buelow JU et al (2018) Patient characteristics and predictors of return to sport at 12 months after anterior cruciate ligament reconstruction: the importance of patient age and postoperative rehabilitation. Orthop J Sports Med 6:2325967118797575
Collins NJ, Prinsen CA, Christensen R, Bartels EM, Terwee CB, Roos EM (2016) Knee Injury and Osteoarthritis Outcome Score (KOOS): systematic review and meta-analysis of measurement properties. Osteoarthr Cartil 24:1317–1329
Higgins LD, Taylor MK, Park D, Ghodadra N, Marchant M, Pietrobon R et al (2007) Reliability and validity of the international knee documentation committee (IKDC) subjective knee form. Jt Bone Spine 74:594–599
Lunn TH, Kristensen BB, Andersen L, Husted H, Otte KS, Gaarn-Larsen L et al (2011) Effect of high-dose preoperative methylprednisolone on pain and recovery after total knee arthroplasty: a randomized, placebo-controlled trial. Br J Anaesth 106:230–238
Kampitak W, Tanavalee A, Ngarmukos S, Amarase C (2019) Opioid-sparing analgesia and enhanced recovery after total knee arthroplasty using combined triple nerve blocks with local infiltration analgesia. J Arthroplasty 34:295–302
Andersen L, Kehlet H (2014) Analgesic efficacy of local infiltration analgesia in hip and knee arthroplasty: a systematic review. Br J Anaesth 113:360–374
Funding
There is no funding source.
Author information
Authors and Affiliations
Contributions
YL: study design, data acquisition, data analysis, data interpretation, manuscript drafting, and critical revision. EF: study design, data acquisition, data analysis, data interpretation, manuscript drafting, and critical revision. RRW: study design, data acquisition, data analysis, data interpretation, manuscript drafting, and critical revision. OLG: study design, data acquisition, data analysis, data interpretation, manuscript drafting, and critical revision. MCF: study design, data interpretation, manuscript drafting, and critical revision. ABY: study design, data interpretation, manuscript drafting, and critical revision. BJC: study design, data interpretation, manuscript drafting, and critical revision. NV: study design, data interpretation, manuscript drafting, and critical revision. BF: study design, data acquisition, data analysis, data interpretation, manuscript drafting, and critical revision.
Corresponding author
Ethics declarations
Conflict of interest
M.C.F. reports grants from Arthrex, Inc., grants from ACUMED LLC, other from EXACTECH, INC, other from ENCORE MEDICAL, LP, other from Stryker Corporation, other from Vericel Corporation, other from Zimmer Biomet Holdings, Inc., other from DePuy Synthes Sales Inc., outside the submitted work; and Arthroscopy: Editorial or governing board, DJ Orthopaedics: Paid presenter or speaker, HSS Journal: Editorial or governing board. A.B.Y. reports personal fees and other from Joint Restoration Foundation, Inc., personal fees from Olympus America, Inc., non-financial support from Medwest Associates, other from Smith + Nephew, Inc., other from Aesculap Biologics, LLC, personal fees from CONMED, other from Arthrex, Inc, other from Organogenesis, other from Patient IQ, other from Vericel, outside the submitted work. B.J.C reports personal fees from Arthrex, Inc., personal fees from Anika Therapeutics, Inc., personal fees from DJO, LLC, other from Stryker Corporation, other from Aastrom Biosciences, Inc, other from Smith & Nephew, Inc, other from Depuy Orthopaedics Inc., personal fees and other from LifeNet Health Inc., personal fees from zimmer biomet holdings, other from Geistlich Pharma, North America, Inc., other from CyMedica Orthopedics, Inc, other from Ceterix Orthopaedics, Inc., other from Vericel Corporation, personal fees from Cartiva, Inc., other from GE Healthcare, personal fees from ACUMED LLC, personal fees from Flexion Therapeutics, Inc., other from Aesculap/B.Braun, other from Athletico, personal fees from Elsevier Publishing, other from NIH, other from Operative Techniques in Sport Medicine, other from Ossio, personal fees from Regentis, outside the submitted work; and American Journal of Orthopedics: Editorial or governing board, American Journal of Sports Medicine: Editorial or governing board, Arthroscopy Association of North America: Board or committee member, Cartilage: Editorial or governing board, International Cartilage Repair Society: Board or committee member, Journal of Shoulder and Elbow Surgery: Editor only: Editorial or governing board, Journal of the American Academy of Orthopaedic Surgeons: Editor only: Editorial or governing board. N.V. reports personal fees from Smith + Nephew, Inc, personal fees from Styker Corporation, other from Relievant Medsystems, Inc, other from DePuy Synthes Sales Inc., other from Vericel Corporation, personal fees from Medacta USA, Inc, other from Athroscopy, other from Breg, other from Cymedica, personal fees and other from Minivasive, other from Omeros, personal fees from Orthospace, other from Ossur, other from Vindico Medical-Orthopedics Hyperguide, other from Wright Medical Technology, Inc., outside the submitted work; and American Orthopaedic Society for Sports Medicine: Board or committee member, American Shoulder and Elbow Surgeons: Board or committee member, Arthroscopy Association of North America: Board or committee member, Knee: Editorial or governing board, SLACK Incorporated: Editorial or governing board. B.F. reports research support from Arthrex and Stryker; educational support from Medwest, Smith & Nephew, and Ossur; consulting fees from Arthrex, DJO, Smith & Nephew, Ossur, Sonoma Orthopedics, and Stryker; speaking fees from Arthrex; honoraria from Arthrosurface; and royalties from Elsevier and Arthrex; and has stock options in Jace Medical.
Ethical approval
This study utilized previously collected data from an institutional database. The present study was granted IRB exemption by the IRB at Rush University and was adherent to all ethical standards put forth by IRB at Rush University.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lu, Y., Forlenza, E., Wilbur, R.R. et al. Machine-learning model successfully predicts patients at risk for prolonged postoperative opioid use following elective knee arthroscopy. Knee Surg Sports Traumatol Arthrosc 30, 762–772 (2022). https://doi.org/10.1007/s00167-020-06421-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06421-7