Abstract
Purpose
No studies have been conducted to determine long-term predictors of clinical failure after surgical root repair. This study identified long-term prognostic factors of clinical failure after pull-out repair of medial meniscus posterior root tears (MMPRTs) at a minimum of 10 year follow-up.
Methods
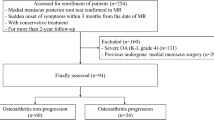
A total of 37 patients who underwent MMPRT pull-out repair and had been observed for more than 10 years were recruited for this study. The mean follow-up period was 125.9 ± 21.2 months. Clinical failure of the procedures was defined as conversion to total knee arthroplasty (TKA). Participants were categorized into two groups: non-failure and failure groups. Various factors, including demographic features and radiologic findings, were analyzed and compared between the two groups. Meniscus extrusion was assessed at coronal magnetic resonance imaging preoperatively and 1 year postoperatively. Independent risk factors were determined by univariate analysis and logistic regression analysis. To determine the cut-off value for risk factors, the receiver-operating characteristic curve analysis was performed.
Results
In total, eight patients (22%) were converted to TKA during the follow-up period. With univariate analysis, statistically significant differences between two groups were observed in mechanical varus alignment (P = 0.018), rate of the number of patient with more meniscal extrusion values after surgery (P = 0.024), and the difference between the preoperative and 1-year postoperative value of meniscus extrusion (mm) (P = 0.010). In a logistic analysis, OR of mechanical varus alignment and differences in meniscus extrusion value before and 1 year after surgery was 1.5 (P = 0.048) and 3.7 (P = 0.034). The cut-off values of mechanical varus alignment and differences in meniscus extrusion values were 5 degrees and 0.7 mm.
Conclusion
Clinically, preoperative varus alignment and increased meniscal extrusion after surgery were found to be predictive for a clinical failure after meniscal root repair in a long-term perspective. Thus, these negative prognostic factors should be taken into consideration for performing root repair in MMPRTs.
Level of evidence
Level III.

Similar content being viewed by others
References
Allaire R, Muriuki M, Gilbertson L, Harner CD (2008) Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am 90:1922–1931
Bhatia S, LaPrade CM, Ellman MB, LaPrade RF (2014) Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med 42:3016–3030
Cameron ML, Briggs KK, Steadman JR (2003) Reproducibility and reliability of the outerbridge classification for grading chondral lesions of the knee arthroscopically. Am J Sports Med 31:83–86
Chung KS, Choi CH, Bae TS, Ha JK, Jun DJ, Wang JH, Kim JG (2018) Comparison of tibiofemoral contact mechanics after various transtibial and all-inside fixation techniques for medial meniscus posterior root radial tears in a porcine model. Arthroscopy 34:1060–1068
Chung KS, Ha JK, Ra HJ, Kim JG (2016) Arthroscopic medial meniscus posterior root fixation using a modified mason-allen stitch. Arthrosc Tech 5:e63-66
Chung KS, Ha JK, Ra HJ, Kim JG (2016) A meta-analysis of clinical and radiographic outcomes of posterior horn medial meniscus root repairs. Knee Surg Sports Traumatol Arthrosc 24:1455–1468
Chung KS, Ha JK, Ra HJ, Kim JG (2016) Prognostic factors in the midterm results of pullout fixation for posterior root tears of the medial meniscus. Arthroscopy 32:1319–1327
Chung KS, Ha JK, Ra HJ, Nam GW, Kim JG (2017) Pullout fixation of posterior medial meniscus root tears: correlation between meniscus extrusion and midterm clinical results. Am J Sports Med 45:42–49
Chung KS, Ha JK, Ra HJ, Yu WJ, Kim JG (2020) Root repair versus partial meniscectomy for medial meniscus posterior root tears: comparison of long-term survivorship and clinical outcomes at minimum 10-year follow-up. Am J Sports Med. https://doi.org/10.1177/0363546520920561
Chung KS, Ha JK, Yeom CH, Ra HJ, Jang HS, Choi SH, Kim JG (2015) Comparison of clinical and radiologic results between partial meniscectomy and refixation of medial meniscus posterior root tears: a minimum 5-year follow-up. Arthroscopy 31:1941–1950
Feucht MJ, Kuhle J, Bode G, Mehl J, Schmal H, Sudkamp NP, Niemeyer P (2015) Arthroscopic transtibial pullout repair for posterior medial meniscus root tears: a systematic review of clinical, radiographic, and second-look arthroscopic results. Arthroscopy 31:1808–1816
Furumatsu T, Okazaki Y, Kodama Y, Okazaki Y, Kamatsuki Y, Masuda S, Hiranaka T, Ozaki T (2019) The accuracy of a newly developed guide system in medial meniscus posterior root repair: a comparison between two aiming guides. Knee Surg Relat Res 31:7
Han SB, Shetty GM, Lee DH, Chae DJ, Seo SS, Wang KH, Yoo SH, Nha KW (2010) Unfavorable results of partial meniscectomy for complete posterior medial meniscus root tear with early osteoarthritis: a 5- to 8-year follow-up study. Arthroscopy 26:1326–1332
Jung YH, Choi NH, Oh JS, Victoroff BN (2012) All-inside repair for a root tear of the medial meniscus using a suture anchor. Am J Sports Med 40:1406–1411
Kang DG, Park YJ, Yu JH, Oh JB, Lee DY (2019) A systematic review and meta-analysis of arthroscopic meniscus repair in young patients: comparison of all-inside and inside-out suture techniques. Knee Surg Relat Res 31:1–11
Kennedy MI, Strauss M, LaPrade RF (2020) Injury of the meniscus root. Clin Sports Med 39:57–68
Kim DH, Lee GC, Kim HH, Cha DH (2020) Correlation between meniscal extrusion and symptom duration, alignment, and arthritic changes in medial meniscus posterior root tear: research article. Knee Surg Relat Res 32:2
Kim SB, Ha JK, Lee SW, Kim DW, Shim JC, Kim JG, Lee MY (2011) Medial meniscus root tear refixation: comparison of clinical, radiologic, and arthroscopic findings with medial meniscectomy. Arthroscopy 27:346–354
Kodama Y, Furumatsu T, Kamatsuki Y, Hiranaka T, Takahata T, Sadakane M, Ikuta H, Yasumitsu M, Ozaki T (2019) Preliminary diagnosis of medial meniscus posterior root tears using the Rosenberg radiographic view. Knee Surg Relat Res 31:9
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15:155–163
Krych AJ, Johnson NR, Mohan R, Dahm DL, Levy BA, Stuart MJ (2018) Partial meniscectomy provides no benefit for symptomatic degenerative medial meniscus posterior root tears. Knee Surg Sports Traumatol Arthrosc 26:1117–1122
LaPrade CM, Foad A, Smith SD, Turnbull TL, Dornan GJ, Engebretsen L, Wijdicks CA, LaPrade RF (2015) Biomechanical consequences of a nonanatomic posterior medial meniscal root repair. Am J Sports Med 43:912–920
Lee DW, Kim MK, Jang HS, Ha JK, Kim JG (2014) Clinical and radiologic evaluation of arthroscopic medial meniscus root tear refixation: comparison of the modified Mason-Allen stitch and simple stitches. Arthroscopy 30:1439–1446
Lee HI, Park D, Cho J (2018) Clinical and radiological results with second-look arthroscopic findings after open wedge high tibial osteotomy without arthroscopic procedures for medial meniscal root tears. Knee Surg Relat Res 30:34–41
Lee JH, Lee DH, Park JH, Suh DW, Kim E, Jang KM (2020) Poorer dynamic postural stability in patients with anterior cruciate ligament rupture combined with lateral meniscus tear than in those with medial meniscus tear. Knee Surg Relat Res 32:8
Lee YG, Shim JC, Choi YS, Kim JG, Lee GJ, Kim HK (2008) Magnetic resonance imaging findings of surgically proven medial meniscus root tear: tear configuration and associated knee abnormalities. J Comput Assist Tomogr 32:452–457
Matthews JR, Wang J, Zhao J, Kluczynski MA, Bisson LJ (2020) The influence of suture materials on the biomechanical behavior of suture-meniscal specimens: a comparative study in a porcine model. Knee Surg Relat Res 32:42
Moon HK, Koh YG, Kim YC, Park YS, Jo SB, Kwon SK (2012) Prognostic factors of arthroscopic pull-out repair for a posterior root tear of the medial meniscus. Am J Sports Med 40:1138–1143
Navarro RA, Adams AL, Lin CC, Fleming J, Garcia IA, Lee J, Black MH (2020) Does knee arthroscopy for treatment of meniscal damage with osteoarthritis delay knee replacement compared to physical therapy alone? Clin Orthop Surg 12:304–311
Okazaki Y, Furumatsu T, Shimamura Y, Saiga K, Ohashi H, Uchino T, Kamatsuki Y, Okazaki Y, Ozaki T (2019) Time-dependent increase in medial meniscus extrusion after medial meniscus posterior root tear analyzed by using magnetic resonance imaging. Knee Surg Relat Res 31:120–125
Ozkoc G, Circi E, Gonc U, Irgit K, Pourbagher A, Tandogan RN (2008) Radial tears in the root of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc 16:849–854
Padalecki JR, Jansson KS, Smith SD, Dornan GJ, Pierce CM, Wijdicks CA, Laprade RF (2014) Biomechanical consequences of a complete radial tear adjacent to the medial meniscus posterior root attachment site: in situ pull-out repair restores derangement of joint mechanics. Am J Sports Med 42:699–707
Robertson DD, Armfield DR, Towers JD, Irrgang JJ, Maloney WJ, Harner CD (2009) Meniscal root injury and spontaneous osteonecrosis of the knee: an observation. J Bone Joint Surg Br 91:190–195
Seo HS, Lee SC, Jung KA (2011) Second-look arthroscopic findings after repairs of posterior root tears of the medial meniscus. Am J Sports Med 39:99–107
Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD (2001) The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA 286:188–195
Shelbourne KD, Dickens JF (2006) Digital radiographic evaluation of medial joint space narrowing after partial meniscectomy of bucket-handle medial meniscus tears in anterior cruciate ligament-intact knees. Am J Sports Med 34:1648–1655
Sood M, Kulshrestha V, Sachdeva J, Ghai A, Sud A, Singh S (2020) Poor functional outcome in patients with voluntary knee instability after anterior cruciate ligament reconstruction. Clin Orthop Surg 12:312–317
Walter SD, Eliasziw M, Donner A (1998) Sample size and optimal designs for reliability studies. Stat Med 17:101–110
Acknowledgements
All authors have no potential conflict of interest, including financial interests, activities, relationships, and affiliations, to disclose.
Funding
All authors declare that this study had no funding resource.
Author information
Authors and Affiliations
Contributions
KSC and JGK designed the study. JKH and HJR analyzed the data and performed the calculations. KSC, JKH, and HJR performed formal analysis. KSC wrote the manuscript with input from the all authors. All authors provided critical feedback and helped shape the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study protocol was reviewed and approved by the Institutional Review Board (IRB) of our institute (IRB no. PAIK-2020-02-012).
Informed consent
The Institutional Review Board (IRB) waived the requirements of informed consent as all data were anonymous. Therefore, this study was performed without prior informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chung, K.S., Ha, J.K., Ra, H.J. et al. Preoperative varus alignment and postoperative meniscus extrusion are the main long-term predictive factors of clinical failure of meniscal root repair. Knee Surg Sports Traumatol Arthrosc 29, 4122–4130 (2021). https://doi.org/10.1007/s00167-020-06405-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06405-7