Abstract
Purpose
A medial meniscus posterior root tear results in the loss of meniscal circumferential hoop stress and causes a pathological posteromedial extrusion of the medial meniscus. Although creating a tibial tunnel in the anatomic place improves postoperative medial meniscus posterior extrusion, no studies have evaluated the relationship between tibial tunnel position and clinical outcomes. This study aimed to evaluate how tibial tunnel positioning of medial meniscus posterior root pullout repair affects meniscal healing status and clinical outcomes.
Methods
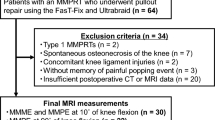
Sixty-two patients with 64 medial meniscus posterior root tears (mean age 62.8 ± 7.9 years) who had undergone pullout repairs and second-look arthroscopies were included. All 62 patients were Lachman test negative. Three-dimensional computed tomography images of the tibial surface were evaluated using a rectangular measurement grid to assess the tibial tunnel centre and medial meniscus posterior root attachment centre. Spearman’s rank correlation analysis was undertaken to determine displacement distance from the medial meniscus posterior root attachment centre to the tibial tunnel centre and a meniscal healing score, as well as clinical outcomes at 1 year post-repair.
Results
Tibial tunnel centres were located more anteriorly and medially than the medial meniscus posterior root attachment centre (mean distance 5.0 ± 2.2 mm). The mean meniscal healing score was 6.7 ± 1.8 of 10 possible points. The 1-year postoperative clinical scores showed significant improvement compared with preoperative scores for all the items. There was a significant negative correlation in the absolute distance between the medial meniscus posterior root attachment centre and the tibial tunnel centre with the meniscal healing score (ρ = − 0.39, p = 0.002). Furthermore, there were significant positive correlations between the distance between the medial meniscus posterior root attachment centre and the tibial tunnel centre in the mediolateral direction and patient-based clinical outcomes (ρ = 0.25–0.43, p < 0.05).
Conclusion
Accurate placement of a tibial tunnel, especially in the mediolateral direction, significantly improved meniscal healing and clinical outcomes at 1 year following medial meniscus posterior root repair. Surgeons should create a medial meniscus posterior root tibial tunnel at the anatomic attachment with particular attention to the mediolateral position.
Level of evidence
Level IV.



Similar content being viewed by others
Abbreviations
- Ac:
-
Attachment centre
- ACL:
-
Anterior cruciate ligament
- AP:
-
Anteroposterior
- BMI:
-
Body mass index
- CT:
-
Computed tomography
- F-MMA:
-
FasT-Fix modified Mason–Allen suture
- FTA:
-
Femorotibial angle
- ICC:
-
Intra-class correlation coefficient
- IKDC:
-
International Knee Documentation Committee
- K–L:
-
Kellgren–Lawrence
- KOOS:
-
Knee Injury and Osteoarthritis Outcome Score
- ML:
-
Mediolateral
- MM:
-
Medial meniscus
- MMPRT:
-
Medial meniscus posterior root tear
- MRI:
-
Magnetic resonance imaging
- MTE:
-
Medial tibial eminence
- OA:
-
Osteoarthritis
- OATS:
-
Osteochondral autograft transplantation surgery
- QOL:
-
Knee-related quality of life
- SD:
-
Standard deviation
- SIFK:
-
Subchondral insufficiency fracture of the knee
- SONK:
-
Spontaneous osteonecrosis of the knee
- Tc:
-
Tibial tunnel centre
- TSS:
-
Two simple stitches
- VAS:
-
Visual analogue scale
- 3D:
-
Three-dimensional
References
Allaire R, Muriuki M, Gilbertson L, Harner CD (2008) Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am 90:1922–1931
Bae JH, Paik NH, Park GW, Yoon JR, Chae DJ, Kwon JH et al (2013) Predictive value of painful popping for a posterior root tear of the medial meniscus in middle-aged to older Asian patients. Arthroscopy 29:545–549
Brophy RH, Wojahn RD, Lillegraven O, Lamplot JD (2019) Outcomes of arthroscopic posterior medial meniscus root repair: association with body mass index. J Am Acad Orthop Surg 27:104–111
Chung KS, Ha JK, Ra HJ, Yu WJ, Kim JG (2020) Root repair versus partial Meniscectomy for medial meniscus posterior root tears: comparison of long-term survivorship and clinical outcomes at minimum 10-year follow-up. Am J Sports Med 48:1937–1944
Daney BT, Aman ZS, Krob JJ, Storaci HW, Brady AW, Nakama G et al (2019) Utilization of transtibial centralization suture best minimizes extrusion and restores tibiofemoral contact mechanics for anatomic medial meniscal root repairs in a cadaveric model. Am J Sports Med 47:1591–1600
Dürselen L, Vögele S, Seitz AM, Ignatius A, Friederich NF, Bauer G et al (2011) Anterior knee laxity increases gapping of posterior horn medial meniscal tears. Am J Sports Med 39:1749–1755
Fujii M, Furumatsu T, Kodama Y, Miyazawa S, Hino T, Kamatsuki Y et al (2017) A novel suture technique using the FasT-Fix combined with Ultrabraid for pullout repair of the medial meniscus posterior root tear. Eur J Orthop Surg Traumatol 27:559–562
Furumatsu T, Kodama Y, Fujii M, Tanaka T, Hino T, Kamatsuki Y et al (2017) A new aiming guide can create the tibial tunnel at favorable position in transtibial pullout repair for the medial meniscus posterior root tear. Orthop Traumatol Surg Res 103:367–371
Furumatsu T, Miyazawa S, Fujii M, Tanaka T, Kodama Y, Ozaki T (2019) Arthroscopic scoring system of meniscal healing following medial meniscus posterior root repair. Int Orthop 43:1239–1245
Furumatsu T, Okazaki Y, Kodama Y, Okazaki Y, Kamatsuki Y, Masuda S et al (2019) The accuracy of a newly developed guide system in medial meniscus posterior root repair: a comparison between two aiming guides. Knee Surg Relat Res 31:7
Hagmeijer MH, Hevesi M, Desai VS, Sanders TL, Camp CL, Hewett TE et al (2019) Secondary meniscal tears in patients with anterior cruciate ligament injury: relationship among operative management, osteoarthritis, and arthroplasty at 18-year mean follow-up. Am J Sports Med 47:1583–1590
Henning CE, Lynch MA, Yearout KM, Vequist SW, Stallbaumer RJ, Decker KA (1990) Arthroscopic meniscal repair using an exogenous fibrin clot. Clin Orthop Relat Res 252:64–72
Hino T, Furumatsu T, Miyazawa S, Fujii M, Kodama Y, Kamatsuki Y et al (2020) A histological study of the medial meniscus posterior root tibial insertion. Connect Tissue Res 61:546–553
Hiranaka T, Furumatsu T, Kamatsuki Y, Miyazawa S, Okazaki Y, Masuda S et al (2020) The distance between the tibial tunnel aperture and meniscal root attachment is correlated with meniscal healing status following transtibial pullout repair for medial meniscus posterior root tear. Knee 27:899–905
Inoue H, Furumatsu T, Miyazawa S, Fujii M, Kodama Y, Ozaki T (2018) Improvement in the medial meniscus posterior shift following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 26:434–441
Johannsen AM, Civitarese DM, Padalecki JR, Goldsmith MT, Wijdicks CA, LaPrade RF (2012) Qualitative and quantitative anatomic analysis of the posterior root attachments of the medial and lateral menisci. Am J Sports Med 40:2342–2347
Kamatsuki Y, Furumatsu T, Hiranaka T, Okazaki Y, Okazaki Y, Kodama Y et al (2020) Placement of an anatomic tibial tunnel significantly improves the medial meniscus posterior extrusion at 90 degrees of knee flexion following medial meniscus posterior root pullout repair. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06070-w
Kamatsuki Y, Furumatsu T, Miyazawa S, Kodama Y, Hino T, Okazaki Y et al (2019) The early arthroscopic pullout repair of medial meniscus posterior root tear is more effective for reducing medial meniscus extrusion. Acta Med Okayama 73:503–510
Kellgren JHLJ (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502
Kobayashi M, Watanabe N, Oshima Y, Kajikawa Y, Kawata M, Kubo T (2005) The fate of host and graft cells in early healing of bone tunnel after tendon graft. Am J Sports Med 33:1892–1897
Kodama Y, Furumatsu T, Masuda S, Okazaki Y, Kamatsuki Y, Okazaki Y et al (2019) Transtibial fixation for medial meniscus posterior root tear reduces posterior extrusion and physiological translation of the medial meniscus in middle-aged and elderly patients. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05810-x
LaPrade CM, Foad A, Smith SD, Turnbull TL, Dornan GJ, Engebretsen L et al (2015) Biomechanical consequences of a nonanatomic posterior medial meniscal root repair. Am J Sports Med 43:912–920
LaPrade CM, James EW, Cram TR, Feagin JA, Engebretsen L, LaPrade RF (2015) Meniscal root tears: a classification system based on tear morphology. Am J Sports Med 43:363–369
Masuda S, Furumatsu T, Okazaki Y, Kodama Y, Hino T, Kamatsuki Y et al (2018) Medial meniscus posterior root tear induces pathological posterior extrusion of the meniscus in the knee-flexed position: an open magnetic resonance imaging analysis. Orthop Traumatol Surg Res 104:485–489
Okazaki Y, Furumatsu T, Kodama Y, Kamatsuki Y, Masuda S, Ozaki T (2019) Description of a surgical technique of medial meniscus root repair: a fixation technique with two simple stiches under an expected initial tension. Eur J Orthop Surg Traumatol 29:705–709
Okazaki Y, Furumatsu T, Kodama Y, Kamatsuki Y, Okazaki Y, Hiranaka T et al (2019) Steep posterior slope and shallow concave shape of the medial tibial plateau are risk factors for medial meniscus posterior root tears. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05590-4
Okazaki Y, Furumatsu T, Miyazawa S, Kodama Y, Kamatsuki Y, Hino T et al (2019) Meniscal repair concurrent with anterior cruciate ligament reconstruction restores posterior shift of the medial meniscus in the knee-flexed position. Knee Surg Sports Traumatol Arthrosc 27:361–368
Okazaki Y, Furumatsu T, Miyazawa S, Masuda S, Okazaki Y, Hiranaka T et al (2019) A novel suture technique to reduce the meniscus extrusion in the pullout repair for medial meniscus posterior root tears. Eur J Orthop Surg Traumatol 29:1805–1809
Okazaki Y, Furumatsu T, Okazaki Y, Masuda S, Hiranaka T, Kodama Y et al (2020) Medial meniscus posterior root repair decreases posteromedial extrusion of the medial meniscus during knee flexion. Knee 27:132–139
Okazaki Y, Furumatsu T, Yamaguchi T, Kodama Y, Kamatsuki Y, Masuda S et al (2020) Medial meniscus posterior root tear causes swelling of the medial meniscus and expansion of the extruded meniscus: a comparative analysis between 2D and 3D MRI. Knee Surg Sports Traumatol Arthrosc 28:3405–3415
Okazaki Y, Furumatsu T, Yamauchi T, Okazaki Y, Kamatsuki Y, Hiranaka T et al (2020) Medial meniscus posterior root repair restores the intra-articular volume of the medial meniscus by decreasing posteromedial extrusion at knee flexion. Knee Surg Sports Traumatol Arthrosc 28:3435–3442
Pache S, Aman ZS, Kennedy M, Nakama GY, Moatshe G, Ziegler C et al (2018) Meniscal root tears: current concepts review. Arch Bone Joint Surg 6:250–259
Padalecki JR, Jansson KS, Smith SD, Dornan GJ, Pierce CM, Wijdicks CA et al (2014) Biomechanical consequences of a complete radial tear adjacent to the medial meniscus posterior root attachment site: in situ pull-out repair restores derangement of joint mechanics. Am J Sports Med 42:699–707
Stärke C, Kopf S, Gröbel KH, Becker R (2010) The effect of a nonanatomic repair of the meniscal horn attachment on meniscal tension: a biomechanical study. Arthroscopy 26:358–365
Stone JA, Perrone GS, Nezwek TA, Cui Q, Vlad SC, Richmond JC et al (2019) Delayed ACL reconstruction in patients ≥40 years of age is associated with increased risk of medial meniscal injury at 1 year. Am J Sports Med 47:584–589
Tsukada H, Ishibashi Y, Tsuda E, Fukuda A, Toh S (2008) Anatomical analysis of the anterior cruciate ligament femoral and tibial footprints. J Orthop Sci 13:122–129
Yu H, Adesida AB, Jomha NM (2015) Meniscus repair using mesenchymal stem cells—a comprehensive review. Stem Cell Res Ther 6:86
Acknowledgements
We would like to thank our colleagues for their clinical supports. We would also like to thank Editage (www.editage.jp) for English language editing.
Funding
There is no funding source.
Author information
Authors and Affiliations
Contributions
YKa, TF, and TO designed the study and prepared the manuscript. TF performed the surgeries. YKa reviewed the medical records. YO and KK performed the radiographic evaluations. YKo and TH conducted the measurement of 3D CT images. All the authors have read and approved the final version of the manuscript submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the institutional review board of Okayama University Graduate School (ID number: 1857).
Informed consent
All patients provided informed consent prior to participation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kamatsuki, Y., Furumatsu, T., Hiranaka, T. et al. Accurate placement of a tibial tunnel significantly improves meniscal healing and clinical outcomes at 1 year after medial meniscus posterior root repair. Knee Surg Sports Traumatol Arthrosc 29, 3715–3723 (2021). https://doi.org/10.1007/s00167-020-06376-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06376-9