Abstract
Purpose
The shoulder is the most commonly injured body part in CrossFit training. The aim of this study is to report the clinical and MRI results of an arthroscopic repair of supraspinatus tear associated with SLAP lesion in competitive CrossFit athletes.
Methods
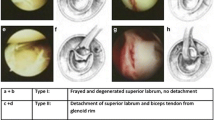
Competitive CrossFit athletes affected by a full-thickness supraspinatus tear associated with SLAP lesion secondary to training injury were prospectively enrolled in the study. Clinical diagnosis was confirmed with MRI (> 1.5 T). Functional evaluation was done using the Constant Score (CS) and ASES score (ASES). All lesions were treated with single-row repair and biceps tenodesis. Minimum follow-up (clinical, MRI) was 24 months.
Results
Nineteen patients were available at the final follow-up. The average age was 43-year-old (range 28–52, SD 8), 12 were males and 7 females. Pre-operative CS and ASES were 67 (range 61–77, SD 7) and 71 (range 62–79, SD 5), respectively. At the 24-month follow-up, 19/19 athletes resumed intensive training and 17/19 returned to competitions. CS and ASES rose to 90 (p = 0.039) and 93 (p = 0.04), respectively. At the final follow-up, MRI indicated complete healing of the tendon in 15 (79%) cases and 4 (21%) cases with type II Sugaya repair integrity. Two of the patients of the latter group did not return to their usual training level and showed type II (Kibler) scapular dyskinesis.
Conclusions
Arthroscopic repair of the supraspinatus tendon associated with biceps tenodesis led to a 100% of return-to-CrossFit training and 90% rate of individuals resuming competitions at 24 months of follow-up. MRI showed 15 (79%) cases of complete healing and 4 (21%) cases with type II Sugaya repair integrity; biceps tenodesis clinically failed only in 1 case and the athlete complained of a decrease in the competitions scores and opted to discontinue CrossFit competitions.
Level of evidence
IV.

Similar content being viewed by others
References
Bergeron MF, Nindl BC, Deuster PA et al (2011) Consortium for Health and Military Performance and American College of Sports Medicine consensus paper on extreme conditioning programs in military personnel. Curr Sports Med Rep 10(6):383–389
Cagle PJ Jr, London DA, Gluck MJ, Morel S, Parsons BO (2020) Long head of biceps tenodesis at the superior aspect of the biceps groove: A biomechanical comparison of inlay and onlay techniques. Shoulder Elbow 12(1):12–17
Carbone S, Candela V, Gumina S (2020) High rate of return to crossfit training after arthroscopic management of rotator cuff tear. Orthop J Sports Med 8(4):2325967120911039
Carbone S, Postacchini R, Gumina S (2015) Scapular dyskinesis and SICK syndrome in patients with a chronic type III acromioclavicular dislocation. Results of rehabilitation. Knee Surg Sports Traumatol Arthrosc 23(5):1473–1480
Everhart JS, Poland S, Vajapey SP, Kirven JC, France TJ, Vasileff WK (2020) CrossFit-related hip and groin injuries: a case series. J Hip Preserv Surg 7(1):109–115. https://doi.org/10.1093/jhps/hnz072
Feito Y, Burrows E, Tabb L, Ciesielka KA (2020) Breaking the myths of competition: a cross-sectional analysis of injuries among CrossFit trained participants. BMJ Open Sport Exerc Med 6(1):e000750. https://doi.org/10.1136/bmjsem-2020-000750
Kibler WB, Sciascia A, Wilkes T (2012) Scapular dyskinesis and its relation to shoulder injury. J Am Acad Orthop Surg 20(6):364–372
Kim DH, Elattrache NS, Tibone JE, Jun BJ, DeLaMora SN, Kvitne RS et al (2006) Biomechanical comparison of a single-row versus double-row suture anchor technique for rotator cuff repair. Am J Sports Med 34:407–414
Mazzocca AD, Millett PJ, Guanche CA, Santangelo SA, Arciero RA (2005) Arthroscopic single-row versus double-row suture anchor rotator cuff repair. Am J Sports Med 5(33):1861–1868
Mehrab M, de Vos RJ, Kraan GA et al (2017) Injury incidence and patterns among Dutch CrossFit athletes. Orthop J Sports Med 5(12):2325967117745263
Merolla G, Chillemi C, Franceschini V, Cerciello S, Ippolito G, Paladini P, Porcellini G (2015) Tendon transfer for irreparable cuff tears: indications and surgical rationale. Muscles Ligaments Tendons J 4(4):425–432
Mihata T, Watanabe C, Fukunishi K, Ohue M, Tsujimura T, Fujiwara K, Kinoshita M (2011) Functional and structural outcomes of single-row versus double-row versus combined double-row and suture-bridge repair for rotator cuff tears. Am J Sports Med 39(10):2091–2098
Motley GS, Guengerich B, Schuller T, Turbyfill A (2018) The Ramp Test: an arthroscopic technique for confirming intra-articular subluxation and instability of the long head of the bicep tendon within the shoulder. Arthrosc Tech 7(4):e327–e330
Snyder SJ (2002) Arthroscopic classification of rotator cuff lesions and surgical decision making Shoulder arthroscopy, 2nd edn. JB Lippincott, Philadelphia, p 204
Sugaya H, Maeda K, Matsuki K, Moriishi J (2007) Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. A prospective outcome study. J Bone Joint Surg Am 89(5):953–960
Szeles PRQ, da Costa TS, da Cunha RA, Hespanhol L, Pochini AC, Ramos LA, Cohen M (2020) CrossFit and the epidemiology of musculoskeletal injuries: a prospective 12-week cohort study. Orthop J Sports Med 8(3):2325967120908884
Warner JP, Krushell RJ, Masquelet A, Gerber C (1992) Anatomy and relationships of the suprascapular nerve: anatomical constraints to mobilization of the supraspinatus and infraspinatus muscles in the management of massive rotator-cuff tears. J Bone Joint Surg Am 74:36–45
Waterman BR, Arroyo W, Heida K, Burks R, Pallis M (2015) SLAP repairs with combined procedures have lower failure rate than isolated repairs in a Military population: Surgical outcomes with minimum 2-year follow-up. Orthop J Sports Med 3(8):2325967115599154. https://doi.org/10.1177/2325967115599154
Weisenthal BM, Beck CA, Maloney MD, DeHaven KE, Giordano BD (2014) Injury rate and patterns among CrossFit athletes. Orthop J Sports Med 2(4):2325967114531177
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was carried out in accordance with the World Medical Association Declaration of Helsinki.
Informed consent
All athletes signed informed consent and were informed about the purpose of the research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Carbone, S., Castagna, V., Passaretti, D. et al. Supraspinatus repair and biceps tenodesis in competitive CrossFit athletes allow for a 100% of return to sport. Knee Surg Sports Traumatol Arthrosc 29, 3929–3935 (2021). https://doi.org/10.1007/s00167-020-06345-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06345-2