Abstract
Purpose
Subchondroplasty® is a novel minimally invasive procedure for painful subchondral bone marrow lesions (BMLs). The aim of this systematic review was to characterize the clinical outcomes of the Subchondroplasty® procedure, a novel minimally invasive procedure for the treatment of BMLs. The hypothesis tested was that patients experience improvements in pain and functional outcomes following the Subchondroplasty® procedure.
Methods
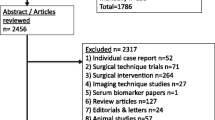
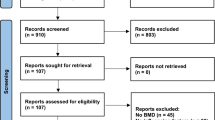
MEDLINE, Embase, Web of Science, and Clinicaltrials.gov were searched from database inception to search date (June 10, 2020) for all clinical studies which discussed Subchondroplasty®. Two reviewers independently screened 45 unique results and 17 studies were included in the final analysis. Data were collected regarding patient demographics, indications, pain, functional scores, conversion to TKA, and complications of the procedure.
Results
All but one study were level IV evidence; the mean MINORS score was 9 ± 2. There were 756 patients included, 45.1% were female, and the mean age was 54 years (range 20–85). Thirteen studies investigated the effect Subchondroplasty® to the knee, while four studied the impact on the foot and ankle. Median length of follow-up was 12 months. The most common indication for Subchondroplasty® was joint pain with corresponding BML. Major contraindications to Subchondroplasty® included severe OA, joint instability, and malalignment. Mean pain score on visual analogue scale (VAS) prior to Subchondroplasty® was 7.8 ± 0.6, but decreased to 3.4 ± 0.7 postoperatively. All studies investigating functional scores reported improvement following Subchondroplasty® (IKDC 31.7 ± 1.9–54.0 ± 4.2 and KOOS 38.1 ± 0.6–70.0 ± 4.1). There were consistently high levels of patient satisfaction; 87 ± 8% of patients would be willing to undergo the procedure again. Seven cases of complications were reported, most seriously osteomyelitis and avascular necrosis. Conversion to knee arthroplasty ranged from 12.5 to 30% with length of follow-up ranging from 10 months to 7 years.
Conclusions
Existing low-quality studies show Subchondroplasty® to benefit patients with BMLs through reduction in pain and improvement in function, along with a high degree of satisfaction following the procedure. The low short-to-medium term conversion rate to arthroplasty suggests that Subchondroplasty® may play a role in delaying more invasive and expensive procedures in patients with BMLs. Subchondroplasty® is a novel procedure that has promising initial findings, but requires further high-quality, comparative studies with long-term follow-up to better understand the outcomes of the procedure and impact clinical practice recommendations.
Level of evidence
Systematic Review of Level III and IV Studies, Level IV.


Similar content being viewed by others
Abbreviations
- BML:
-
Bone marrow lesion
- OA:
-
Osteoarthritis
- VAS:
-
Visual analogue scale
- IKDC:
-
International Knee Documentation Committee
- KOOS:
-
Knee Injury and Osteoarthritis Outcome Score
- MRI:
-
Magnetic resonance imaging
- PRISMA:
-
Preferred Reporting Items for Systematic review and Meta-Analysis
- MINORS:
-
Methodological Index for Non-Randomized Studies
- ICC:
-
Intra-class correlation
- CI:
-
Confidence intervals
- WOMAC:
-
Western Ontario and McMaster Universities Arthritis Index
- FAOS:
-
Foot and Ankle Outcome Score
- TKA:
-
Total knee arthroplasty
- CT:
-
Computed tomography
- MCID:
-
Minimal clinically important difference
- SCB:
-
Substantial clinical benefit
References
Astur DC, de Freitas EV, Cabral PB, Morais CC, Pavei BS, Kaleka CC, Debieux P, Cohen M (2019) Evaluation and management of subchondral calcium phosphate injection technique to treat bone marrow lesion. Cartilage 10:395–401
Bonadio MB, Giglio PN, Helito CP, Pécora JR, Camanho GL, Demange MK (2017) Subchondroplasty for treating bone marrow lesions in the knee—initial experience. Rev Bras Ortop 52:325–330
Brimmo OA, Bozynski CC, Cook CR, Kuroki K, Sherman SL, Pfeiffer FM, Stoker AM, Cook JL (2018) Subchondroplasty for the treatment of post-traumatic bone marrow lesions of the medial femoral condyle in a pre-clinical canine model. J Orthop Res 36:2709–2717
Byrd J, Akhavan S, Frank D, DeMeo P (2017) Short and mid-term outcomes of the subchondroplasty procedure for the treatment of bone marrow in patients with knee osteoarthritis. Arthrosc J Arthrosc Relat Surg 33:e32
Chan JJ, Guzman JZ, Vargas L, Myerson CL, Chan J, Vulcano E (2018) Safety and effectiveness of talus subchondroplasty and bone marrow aspirate concentrate for the treatment of osteochondral defects of the talus. Orthopedics 41:E734–E737
Chirichella PS, Malanga G (2017) Treatment of femoral osteonecrotic lesion following failed subchondroplasty with bone marrow aspirate concentrate loaded allograft: a case report. PM&R 9:S220
Chua K, Kang JYB, Ng FDJ, Pang HN, Lie DTT, Silva A, Chang PCC (2019) Subchondroplasty for bone marrow lesions in the arthritic knee results in pain relief and improvement in function. J Knee Surg. https://doi.org/10.1055/s-0039-1700568
Cohen SB, Sharkey PF (2016) Subchondroplasty for treating bone marrow lesions. J Knee Surg 29:555–563
Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, Bridgett L, Williams S, Guillemin F, Hill CL, Laslett LL, Jones G, Cicuttini F, Osborne R, Vos T, Buchbinder R, Woolf A, March L (2014) The global burden of hip and knee osteoarthritis: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis 73:1323–1330
Davis AT, Byrd JM, Zenner JA, Frank DA, DeMeo PJ, Akhavan S (2015) Short-term outcomes of the subchondroplasty procedure for the treatment of bone marrow edema lesions in patients with knee osteoarthritis. Orthop J Sport Med 3(Suppl):2
Dold AP, Perretta D, Youm T (2017) Osteomyelitis after calcium phosphate subchondroplasty: a case report. Bull Hosp Joint Dis 75:282–285
Ekhtiari S, Horner NS, Bedi A, Ayeni OR, Khan M (2018) The learning curve for the latarjet procedure: a systematic review. Orthop J Sport Med. https://doi.org/10.1177/2325967118786930
Farr J, Cohen SB (2013) Expanding applications of the subchondroplasty procedure for the treatment of bone marrow lesions observed on magnetic resonance imaging. Oper Tech Sports Med 21:138–143
Felson DT, McLaughlin S, Goggins J, LaValley MP, Gale ME, Totterman S, Li W, Hill C, Gale D (2003) Bone marrow edema and its relation to progression of knee osteoarthritis. Ann Intern Med 139:330–336
Ghasemi RA, Sadeghi S, Rahimee N, Tahmasebi M (2019) Technologies in the treatment of bone marrow Edema syndrome. Orthop Clin North Am 50:131–138
Hajnik C, Akhavan S, Wyland DJ, Cohen SB, Jazrawi LM, Youm T, Loren GJ, Farr J, Rahme MD, Rahme M, Reischling P (2019) Two year clinical outcomes of the Subchondroplasty® procedure for treatment of symptomatic bone marrow lesions of the knee. Orthop J Sport Med 7(Suppl):5
Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, Welch V (2019) Cochrane Handbook for Systematic Reviews of Interventions version 6.0. Cochrane. Available via www.training.cochrane.org/handbook. Accessed 15 Jun 2020
Hörterer H, Baumbach SF, Gregersen J, Kriegelstein S, Gottschalk O, Szeimies U, Walther M (2018) Treatment of bone marrow edema of the foot and ankle with the prostacyclin Analog Iloprost. Foot Ankle Int 39:1183–1191
Kompel AJ, Roemer FW, Murakami AM, Diaz LE, Crema MD, Guermazi A (2019) Intra-articular Corticosteroid Injections in the Hip and Knee: Perhaps not as safe as we thought? Radiology 293:656–663
Levy AS, Cousins K (2020) The rational for and efficacy of subchondroplasty in the injured worker. J Orthop 22:48–52
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart L, PRISMA-P (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4:1–9
Nevalainen MT, Sharkey PF, Cohen SB, Roedl JB, Zoga AC, Morrison WB (2016) MRI findings of subchondroplasty of the knee: A two-case report. Clin Imaging 40:241–243
Ogura T, Ackermann J, Mestriner AB, Merkely G, Gomoll AH (2018) The minimal clinically important difference and substantial clinical benefit in the patient-reported outcome measures of patients undergoing osteochondral allograft transplantation in the knee. Cartilage. https://doi.org/10.1177/1947603518812552
Previtali D, Merli G, Di Laura FG, Candrian C, Zaffagnini S, Filardo G (2020) The long-lasting effects of “placebo injections” in knee osteoarthritis: a meta-analysis. Cartilage. https://doi.org/10.1177/1947603520906597
Scher C, Craig J, Nelson F (2008) Bone marrow edema in the knee in osteoarthrosis and association with total knee arthroplasty within a three-year follow-up. Skeletal Radiol 37:609–617
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (Minors): development and validation of a new instrument. ANZ J Surg 73:712–716
Taylor C, Casagranda B, Long J, Akhavan S (2017) Can bone marrow Edema predict knee subchondroplasty outcome? Skeletal Radiol 46:415–441
Tubach F, Ravaud P, Baron G, Falissard B, Logeart I, Bellamy N, Bombardier C, Felson D, Hochberg M, Van Der Heijde D, Dougados M (2005) Evaluation of clinically relevant changes in patient reported outcomes in knee and hip osteoarthritis: the minimal clinically important improvement. Ann Rheum Dis 64:29–33
Yang G, Liu J, Li F, Pan Z, Ni X, Shen Y, Xu H, Huang Q (2014) Bioactive calcium sulfate/magnesium phosphate cement for bone substitute applications. Mater Sci Eng C 35:70–76
Yoo JY, O’Malley MJ, Matsen Ko LJ, Cohen SB, Sharkey PF (2016) Knee arthroplasty after subchondroplasty: early results, complications, and technical challenges. J Arthroplasty 31:2188–2192
Yusuf E, Kortekaas MC, Watt I, Huizinga TWJ, Kloppenburg M (2011) Do knee abnormalities visualised on MRI explain knee pain in knee osteoarthritis? A systematic review. Ann Rheum Dis 70:60–67
Funding
No financial contributions were received for this project.
Author information
Authors and Affiliations
Contributions
LNN and MS performed screening and data extraction, assessed study quality, and drafted the manuscript. SE designed the study, carried out the search, and coordinated data extraction and manuscript preparation. DEA, JAG, and MK edited the manuscript and provided key expert input. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Author JAG has received research funding from JRF Ortho, Aesculap Biologics, Arthrex, and consulted for JRF Ortho, Vericel, Conmed Linvatec.
Ethical approval and informed consent
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nairn, L.N., Subramaniam, M., Ekhtiari, S. et al. Safety and early results of Subchondroplasty® for the treatment of bone marrow lesions in osteoarthritis: a systematic review. Knee Surg Sports Traumatol Arthrosc 29, 3599–3607 (2021). https://doi.org/10.1007/s00167-020-06294-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06294-w