Abstract
Purpose
To assess the literature on indications, outcomes, and complications in pediatric patients undergoing all-epiphyseal (AE) anterior cruciate ligament reconstruction (ACLR).
Methods
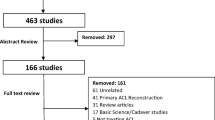
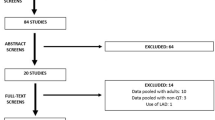
PubMed, Medline, and Embase were searched for literature evaluating AE ACLR in pediatric patients. All included studies were assessed for quality using the Methodological Index for Non-Randomized Studies (MINORS). Descriptive statistics are presented where applicable.
Results
Overall, 17 studies comprising 545 patients, with a mean age of 12.0 ± 1.2 (range 8–19) met the inclusion criteria. The graft choices in this systematic review included hamstring tendon autografts (75.4%, n = 403), quadriceps tendon autograft (6.2%, n = 33), Achilles tendon allograft (3.6%, n = 19) and posterior tibialis tendon allograft in one patient (0.2%, n = 1). Time of return-to-sport ranged from 8 to 22 months. Postoperative subjective IKDC scores were above 90 points. The rate of return-to-sport after AE ACLR was 93.2% (n = 219/235) and 77.9% (n = 142/183) of patients returned to sport at pre-injury level. The overall complication rate was 9.8% (n = 53/545) with the most common complication being ACL re-rupture (5.0%; n = 27/545). Only 1.5% (n = 8/545) of patients demonstrated growth disturbances.
Conclusion
Overall, the AE ACLR technique can achieve good postoperative functional outcomes while notably minimizing the incidence of primary issue of physeal disruption and potential associated leg-length discrepancies. AE ACLR should be considered in pediatric patients with at least 2 years of skeletal growth remaining based on radiographic bone age to minimize the impact of growth-related complications.
Level of evidence
IV (Systematic Review of Level III and IV evidence).

Similar content being viewed by others
Abbreviations
- ACL:
-
Anterior cruciate ligament
- ACLR:
-
Anterior cruciate ligament reconstruction
- AE:
-
All-epiphyseal
- MINORS:
-
Methodological index for non-randomized studies
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-analyses
- R-AMSTAR:
-
Revised Assessment of Multiple Systematic Reviews
- JBJS:
-
Journal of Bone & Joint Surgery
- ICC:
-
Intraclass correlation
- IKDC:
-
International Knee Documentation Committee
- CT:
-
Computed tomography
References
Akinleye SD, Sewick A, Wells L (2013) All-epiphyseal ACL reconstruction: a three-year follow-up. Int J Sports Phys Ther 8(3):300
Anderson CN, Anderson AF (2017) Management of the anterior cruciate ligament-injured knee in the skeletally immature athlete. Clin Sports Med 36(1):35–52
Ardern CL, Ekås GR, Grindem H, Moksnes H, Anderson AF, Chotel F et al (2018) International Olympic Committee consensus statement on prevention, diagnosis and management of paediatric anterior cruciate ligament (ACL) injuries. Br J Sports Med 52(7):422–438
Behr CT, Potter HG, Paletta GA (2001) The relationship of the femoral origin of the anterior cruciate ligament and the distal femoral physeal plate in the skeletally immature knee: an anatomic study. Am J Sports Med 29(6):781–787
Buckle C, Wainwright AM (2018) A systematic review of long-term patient reported outcomes for the treatment of anterior cruciate ligament injuries in the skeletally immature. J Child Orthop 12(3):251–261
Cordasco FA, Black SR, Price M, Wixted C, Heller M, Asaro LA et al (2019) Return to sport and reoperation rates in patients under the age of 20 after primary anterior cruciate ligament reconstruction: risk profile comparing 3 patient groups predicated upon skeletal age. Am J Sports Med 47(3):628–639
Cordasco FA, Mayer SW, Green DW (2017) All-inside, all-epiphyseal anterior cruciate ligament reconstruction in skeletally immature athletes: return to sport, incidence of second surgery, and 2-year clinical outcomes. Am J Sports Med 45(4):856–863
Cruz A, Fabricant P, McGraw M, Rozell J, Ganley T, Wells L (2017) All-epiphyseal ACL reconstruction in children. J Pediatr Orthop 37:204–209
de Sa D, Shanmugaraj A, Weidman M, Peterson D, Simunovic N, Musahl V, Ayeni O (2018) All-inside anterior cruciate ligament reconstruction—a systematic review of techniques, outcomes, and complications. J Knee Surg 31:895–904
Graziano J, Chiaia T, de Mille P, Nawabi DH, Green DW, Cordasco FA (2017) Return to sport for skeletally immature athletes after ACL reconstruction: preventing a second injury using a quality of movement assessment and quantitative measures to address modifiable risk factors. Orthop J Sports Med 5(4):2325967117700599
Greenberg EM, Albaugh J, Ganley TJ, Lawrence JT (2012) Rehabilitation considerations for all epiphyseal ACL reconstruction. Int J Sports Phys Ther 7(2):185
Ho B, Edmonds E, Chambers H, Bastrom T, Pennock A (2018) Risk factors for early ACL reconstruction failure in pediatric and adolescent patients. J Pediatr Orthop 38(7):388–392
Jeon J, Lee J, Kang M (2019) Transphyseal anterior cruciate ligament reconstruction in adolescents with substantial remaining growth causes temporary growth arrest resulting in subclinical leg-length discrepancy. Medicine 98:e16081
Kay J, Memon M, Shah A, Yen YM, Samuelsson K, Peterson D et al (2018) Earlier anterior cruciate ligament reconstruction is associated with a decreased risk of medial meniscal and articular cartilage damage in children and adolescents: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 26(12):3738–3753
Koch PP, Fucentese SF, Blatter SC (2013) Complications after epiphyseal reconstruction of the anterior cruciate ligament in prepubescent children. Knee Surg Sports Traumatol Arthrosc 24(9):2736–2740
Lanzetti R, Pace V, Ciompi A, Perugia D, Spoliti M, Falez F et al (2020) Over the top anterior cruciate ligament reconstruction in patients with open physes: a long-term follow-up study. Int Orthop 44:771–778
Lawrence J, Bowers A, Belding J, Cody S, Ganley T (2010) All-epiphyseal anterior cruciate ligament reconstruction in skeletally immature patients. Clin Orthop Relat Res 468:1971–1977
Lemaitre G, Salle de Chou E, Pineau V, Rochcongar G, Delforge S, Bronfen C et al (2014) ACL reconstruction in children: a transphyseal technique. Orthop Traumatol Surg Res 100:S261–S265
Lykissas M, Nathan S, Wall E (2012) All-epiphyseal anterior cruciate ligament reconstruction in skeletally immature patients: a surgical technique using a split tibial tunnel. Arthrosc Tech 1:e133–e139
McCarthy M, Graziano J, Green D, Cordasco F (2012) All-epiphyseal, all-inside anterior cruciate ligament reconstruction technique for skeletally immature patients. Arthrosc Tech 1:e231–e239
McCarthy M, Tucker S, Nguyen J, Green D, Imhauser C, Cordasco F (2013) Contact stress and kinematic analysis of all-epiphyseal and over-the-top pediatric reconstruction techniques for the anterior cruciate ligament. Am J Sports Med 41:1330–1339
Moher D, Liberati A, Tetzlaff J, Altman D (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097
Nawabi DH, Jones KJ, Lurie B, Potter HG, Green DW, Cordasco FA (2013) Physeal-specific MRI analysis of growth plate disturbance following all-inside anterior cruciate ligament reconstruction in skeletally immature patients: does a physeal-sparing technique offer any advantage? Orthop J Sports Med. https://doi.org/10.1177/2325967113S00025
Patel N, DeFrancesco C, Talathi N, Bram J, Ganley T (2019) All-epiphyseal anterior cruciate ligament reconstruction does not increase the risk of complications compared with pediatric transphyseal reconstruction. J Am Acad Orthop Surg 27:e752–e757
Pennock A, Chambers H, Turk R, Parvanta K, Dennis M, Edmonds E (2018) Use of a modified all-epiphyseal technique for anterior cruciate ligament reconstruction in the skeletally immature patient. Orthop J Sports Med 6:232596711878176
Peterson D, Ayeni O (2016) Pediatric anterior cruciate ligament reconstruction outcomes. Curr Rev Musculoskelet Med 9(4):339–347
Popkin C, Wright M, Pennock A, Vogel L, Padaki A, Redler L et al (2018) Trends in management and complications of anterior cruciate ligament injuries in pediatric patients. J Pediatr Orthop 38:e61–e65
Richter D, Lyon R, Van Valin S, Liu X (2018) Current strategies and future directions to optimize ACL reconstruction in adolescent patients. Front Surg 5:36
Roberti di Sarsina T, Macchiarola L, Signorelli C, Grassi A, Raggi F, Marcheggiani Muccioli G et al (2018) Anterior cruciate ligament reconstruction with an all-epiphyseal “over-the-top” technique is safe and shows low rate of failure in skeletally immature athletes. Knee Surg Sports Traumatol Arthrosc 27:498–506
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg 73(9):712–716
Stanitski C, Harvell J, Fu F (1993) Observations on acute knee hemarthrosis in children and adolescents. J Pediatr Orthop 13(4):506–510
Tuca M, Greditzer H, Gausden E, Uppstrom T, Potter H, Cordasco F et al (2017) Sequential MRI study of graft integrity and signal following pediatric all-epiphyseal ACL reconstruction: does the “sharp turn” at the socket of the distal femoral aperture matter? Orthop J Sports Med. https://doi.org/10.1177/2325967117S00431
Wall EJ, Ghattas PJ, Eismann EA, Myer GD, Carr P (2017) Outcomes and complications after all-epiphyseal anterior cruciate ligament reconstruction in skeletally immature patients. Orthop J Sports Med 5(3):2325967117693604
Wright JG, Swiontkowski MF, Heckman JD (2003) Introducing levels of evidence to the journal. J Bone Jt Surg Br 85-A(1):1–3
Yen Y (2014) Assessment and treatment of knee pain in the child and adolescent athlete. Pediatr Clin N Am 61(6):1155–1173
Funding
There are no potential sources of funding that may influence the writing of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to the writing of this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
The article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gupta, A., Tejpal, T., Shanmugaraj, A. et al. All-epiphyseal anterior cruciate ligament reconstruction produces good functional outcomes and low complication rates in pediatric patients: a systematic review. Knee Surg Sports Traumatol Arthrosc 28, 2444–2452 (2020). https://doi.org/10.1007/s00167-020-06085-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06085-3