Abstract
Purpose
Medial release during total knee arthroplasty (TKA) is used to correct ligament imbalance in knees with varus deformity. However, questions remain on whether residual ligament imbalance would be related to inferior clinical results. The purposes of the present study were to measure the intraoperative joint gap and to evaluate the effect of intraoperative soft tissue condition on the new Knee Society Score (KSS 2011) at 2-year follow-up, without the maneuver of additional medial release to correct the asymmetrical gap balance.
Methods
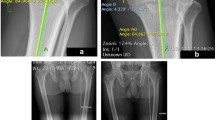
Varus–valgus gap angle and joint gap were measured using a tensor device without medial release for 100 knees with preoperative varus deformity. The knees were categorized according to the varus–valgus gap angle and the laxity. The preoperative and postoperative clinical outcomes using KSS 2011 were compared between the groups.
Results
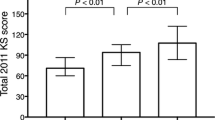
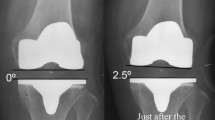
The average varus–valgus angles had a residual imbalance of 2.8° varus and 1.3° varus in extension and flexion, respectively. In comparison, according to varus–valgus joint gap angle and knee laxity in extension and flexion, no significant differences were found in postoperative range of motion and subscale of KSS 2011 among the groups.
Conclusion
Intraoperative asymmetrical joint gap and physiological laxity do not affect early clinical results after TKA.
Level of evidence
III.





Similar content being viewed by others
Abbreviations
- TKA:
-
Total knee arthroplasty
- KSS:
-
Knee Society Score
- MCL:
-
Medial collateral ligament
- SD:
-
Standard deviation
- HKA:
-
Hip–knee–ankle
- FMA:
-
Femoral mechanical angle
- TMA:
-
Tibial mechanical angle
- WOMAC:
-
Western Ontario and McMaster Universities Arthritis Index
References
Akagi M, Oh M, Nonaka T, Tsujimoto H, Asano T, Hamanishi C (2004) An anteroposterior axis of the tibia for total knee arthroplasty. Clin Orthop Relat Res 420:213–219
Asano H, Muneta T, Sekiya I (2008) Soft tissue tension in extension in total knee arthroplasty affects postoperative knee extension and stability. Knee Surg Sports Traumatol Arthrosc 16:999–1003
Aunan E, Kibsgard TJ, Diep LM, Rohrl SM (2015) Intraoperative ligament laxity influences functional outcome 1 year after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 23:1684–1692
Bottros J, Gad B, Krebs V, Barsoum WK (2006) Gap balancing in total knee arthroplasty. J Arthroplasty 21:11–15
Cho WS, Byun SE, Lee SJ, Yoon J (2015) Laxity after complete release of the medial collateral ligament in primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 23:1816–1823
Griffin FM, Insall JN, Scuderi GR (2000) Accuracy of soft tissue balancing in total knee arthroplasty. J Arthroplasty 15:970–973
Hancock GE, Hepworth T, Wembridge K (2018) Accuracy and reliability of knee goniometry methods. J Exp Orthop 5:46
Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclerq V, Hess S (2019) Functional knee phenotypes: a novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surg Sports Traumatol Arthrosc 27:1394–1402
Ismailidis P, Kuster MS, Jost B, Giesinger K, Behrend H (2017) Clinical outcome of increased flexion gap after total knee arthroplasty. Can controlled gap imbalance improve knee flexion? Knee Surg Sports Traumatol Arthrosc 25:1705–1711
Jawhar A, Hutter K, Scharf HP (2016) Outcome in total knee arthroplasty with a medial-lateral balanced versus unbalanced gap. J Orthop Surg (Hong Kong) 24:298–301
Kim MW, Koh IJ, Kim JH, Jung JJ, In Y (2015) Efficacy and safety of a novel three-step medial release technique in varus total knee arthroplasty. J Arthroplasty 30:1542–1547
Koh HS, In Y (2013) Semimembranosus release as the second step of soft tissue balancing in varus total knee arthroplasty. J Arthroplasty 28:273–278
Kuriyama S, Ishikawa M, Nakamura S, Furu M, Ito H, Matsuda S (2016) No condylar lift-off occurs because of excessive lateral soft tissue laxity in neutrally aligned total knee arthroplasty: a computer simulation study. Knee Surg Sports Traumatol Arthrosc 24:2517–2524
Matsumoto T, Muratsu H, Kawakami Y, Takayama K, Ishida K, Matsushita T, Akisue T, Nishida K, Kuroda R, Kurosaka M (2014) Soft-tissue balancing in total knee arthroplasty: cruciate-retaining versus posterior-stabilised, and measured-resection versus gap technique. Int Orthop 38:531–537
Matsumoto T, Takayama K, Muratsu H, Matsushita T, Kuroda R, Kurosaka M (2015) Semimembranosus release reduces tibial internal rotation and flexion angle in cruciate-retaining total knee arthroplasty. J Arthroplasty 30:1537–1541
Meneghini RM, Ziemba-Davis MM, Lovro LR, Ireland PH, Damer BM (2016) Can Intraoperative sensors determine the "Target" ligament balance? Early outcomes in total knee arthroplasty. J Arthroplasty 31:2181–2187
Morcos MW, Lanting BA, Webster J, Howard JL, Bryant D, Teeter MG (2019) Effect of medial soft tissue releases during posterior-stabilized total knee arthroplasty on contact kinematics and patient-reported outcomes. J Arthroplasty 34:1110–1115
Moro-oka TA, Shiraishi H, Iwamoto Y, Banks SA (2010) Modified gap-balancing technique in total knee arthroplasty: evaluation of the post-operative coronal laxity. Knee Surg Sports Traumatol Arthrosc 18:375–380
Nakamura S, Ito H, Kobayashi M, Nakamura K, Toyoji U, Komistek RD, Nakamura T (2014) Are the long term results of a high-flex total knee replacement affected by the range of flexion? Int Orthop 38:761–766
Nakamura S, Ito H, Nakamura K, Kuriyama S, Furu M, Matsuda S (2017) Long-term durability of ceramic tri-condylar knee implants: a minimum 15-year follow-up. J Arthroplasty 32:1874–1879
Nakamura S, Ito H, Yoshitomi H, Kuriyama S, Komistek RD, Matsuda S (2015) Analysis of the flexion gap on in vivo knee kinematics using fluoroscopy. J Arthroplasty 30:1237–1242
Nakamura S, Kobayashi M, Ito H, Nakamura K, Ueo T, Nakamura T (2010) The Bi-Surface total knee arthroplasty: minimum 10-year follow-up study. Knee 17:274–278
Nakamura S, Sharma A, Ito H, Nakamura K, Zingde SM, Komistek RD (2015) Kinematic difference between various geometric centers and contact points for tri-condylar bi-surface knee system. J Arthroplasty 30:701–705
Nakano N, Matsumoto T, Muratsu H, Takayama K, Kuroda R, Kurosaka M (2016) Postoperative knee flexion angle is affected by lateral laxity in cruciate-retaining total knee arthroplasty. J Arthroplasty 31:401–405
Oh CS, Song EK, Seon JK, Ahn YS (2015) The effect of flexion balance on functional outcomes in cruciate-retaining total knee arthroplasty. Arch Orthop Trauma Surg 135:401–406
Okamoto S, Okazaki K, Mitsuyasu H, Matsuda S, Iwamoto Y (2013) Lateral soft tissue laxity increases but medial laxity does not contract with varus deformity in total knee arthroplasty. Clin Orthop Relat Res 471:1334–1342
Okamoto S, Okazaki K, Mitsuyasu H, Matsuda S, Mizu-Uchi H, Hamai S, Tashiro Y, Iwamoto Y (2014) Extension gap needs more than 1-mm laxity after implantation to avoid post-operative flexion contracture in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22:3174–3180
Okazaki K, Miura H, Matsuda S, Takeuchi N, Mawatari T, Hashizume M, Iwamoto Y (2006) Asymmetry of mediolateral laxity of the normal knee. J Orthop Sci 11:264–266
Takayama K, Matsumoto T, Kubo S, Muratsu H, Ishida K, Matsushita T, Kurosaka M, Kuroda R (2012) Influence of intra-operative joint gaps on post-operative flexion angle in posterior cruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20:532–537
Tokuhara Y, Kadoya Y, Nakagawa S, Kobayashi A, Takaoka K (2004) The flexion gap in normal knees. An MRI study. J Bone Jt Surg Br 86:1133–1136
Tsubosaka M, Muratsu H, Takayama K, Miya H, Kuroda R, Matsumoto T (2018) Comparison of intraoperative soft tissue balance between cruciate-retaining and posterior-stabilized total knee arthroplasty performed by a newly developed medial preserving gap technique. J Arthroplasty 33:729–734
Tsukeoka T, Tsuneizumi Y, Yoshino K (2017) The rectangular flexion gap is associated with an increased knee flexion angle in a cruciate-sacrificing rotating platform mobile-bearing total knee arthroplasty. J Orthop Sci 22:313–317
Vanlommel L, Vanlommel J, Claes S, Bellemans J (2013) Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc 21:2325–2330
Watanabe M, Kuriyama S, Nakamura S, Nishitani K, Tanaka Y, Sekiguchi K, Ito H, Matsuda S (2019) Impact of intraoperative adjustment method for increased flexion gap on knee kinematics after posterior cruciate ligament-sacrificing total knee arthroplasty. Clin Biomech (Bristol, Avon) 63:85–94
Whiteside LA, Saeki K, Mihalko WM (2000) Functional medical ligament balancing in total knee arthroplasty. Clin Orthop Relat Res 380:45–57
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Funding
One or more authors (SN and SM) received research grant from Kyocera outside the submitted work.
Ethical approval
The study design was approved by the institutional ethics review boards, and all procedures performed were in accordance with the ethical standards of the institutional research committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tanaka, Y., Nakamura, S., Kuriyama, S. et al. Intraoperative physiological lateral laxity in extension and flexion for varus knees did not affect short-term clinical outcomes and patient satisfaction. Knee Surg Sports Traumatol Arthrosc 28, 3888–3898 (2020). https://doi.org/10.1007/s00167-020-05862-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-05862-4