Abstract
Purpose
The purposes of this study were to investigate the anatomical risk factors of grade 3 J-sign and analyse the influence of J-sign grades on the short-term clinical outcomes of patients with recurrent patellar dislocation.
Methods
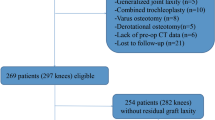
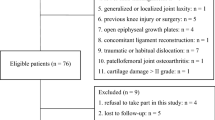
From 2016 to 2018, a total of 168 patients with recurrent patellar dislocation (187 knees) underwent medial patellofemoral ligament reconstruction with or without tibial tuberosity medialization. Pre-operative J-sign severity was graded according to a previously described classification (grades 1–3). Potential anatomical risk factors of J-sign were explored. Comparisons were assessed between patients with different grades of J-sign using univariate and binary logistic regression analyses. The Kujala score was assessed and compared with pre-operative values, and stress fluoroscopy was performed to assess medial patellofemoral ligament residual graft laxity. Among the 130 included cases, 104 knees with at least 1-year follow-up were included in the clinical outcome analyses to explore the influence of several anatomical factors and J-sign grade on short-term clinical outcomes.
Results
A total of 118 patients (130 knees) were included in the present study. The median age at surgery was 21 years (range 13–38), and 111 affected knees belonged to female patients (85%). Univariate and multivariate logistic regressions between the grade 3 group and the grade 1–2 groups showed that increased femoral anteversion, excessive external tibial torsion, and patella alta were three independent risk factors of grade 3 J-sign in patients with recurrent patellar dislocation. A total of 104 knees with at least a 1-year follow-up were included in the clinical outcome analyses. The median Kujala score improved from 54 (range, 38–72) pre-operatively to 86 (range, 70–100) post-operatively. Although no re-dislocation was reported during the follow-up, 6 out of 32 patients in the grade 3 group demonstrated “MPFL residual graft laxity” based on post-operative stress radiography (18.8%), which was significantly higher than in the grade 1–2 groups (0%, p < 0.001). Subgroup analysis showed that patients with grade 3 J-sign had significantly lower post-operative Kujala scores than those with grade 1–2 J-sign (p < 0.001). Moreover, increased femoral anteversion (≥ 30°) was correlated with an inferior post-operative Kujala score (p = 0.023).
Conclusion
The three independent anatomic risk factors of grade 3 J-sign in patients with recurrent patellar dislocation were increased femoral anteversion, excessive external tibial torsion, and patella alta. A pre-operative grade 3 J-sign was correlated with a lower post-operative Kujala score and more “MPFL residual graft laxity” in patients with recurrent patellar dislocation treated with MPFL reconstruction with or without tibial tuberosity medialization at a minimum 1-year follow-up.
Level of evidence
III





Similar content being viewed by others
References
Banke IJ, Kohn LM, Meidinger G, Otto A, Hensler D, Beitzel K et al (2014) Combined trochleoplasty and MPFL reconstruction for treatment of chronic patellofemoral instability: a prospective minimum 2-year follow-up study. Knee Surg Sports Traumatol Arthrosc 22(11):2591–2598
Biyani R, Elias JJ, Saranathan A, Feng H, Guseila LM, Morscher MA et al (2014) Antomical factors influencing patellar tracking in the unstable patellofemoral joint. Knee Surg Sports Traumatol Arthrosc 22(10):2334–2341
Blond L, Haugegaard M (2014) Combined arthroscopic deepening trochleoplasty and reconstruction of the medial patellofemoral ligament for patients with recurrent patella dislocation and trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc 22(10):2484–2490
Bouras T, Brown A, Gallacher P, Barnett A (2019) Isolated medial patellofemoral ligament reconstruction significantly improved quality of life in patients with recurrent patella dislocation. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05447-w
Camp CL, Stuart MJ, Krych AJ, Levy BA, Bond JR, Collins MS et al (2013) CT and MRI measurements of tibial tubercle-trochlear groove distances are not equivalent in patients with patellar instability. Am J Sports Med 41(8):1835–1840
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2(1):19–26
Dickschas J, Harrer J, Pfefferkorn R, Strecker W (2012) Operative treatment of patellofemoral maltracking with torsional osteotomy. Arch Orthop Trauma Surg 132(3):289–298
Diederichs G, Köhlitz T, Kornaropoulos E, Heller MO, Vollnberg B, Scheffler S (2013) Magnetic resonance imaging analysis of rotational alignment in patients with patellar dislocations. Am J Sports Med 41(1):51–57
Erkocak OF, Altan E, Altintas M, Turkmen F, Aydin BK, Bayar A (2016) Lower extremity rotational deformities and patellofemoral alignment parameters in patients with anterior knee pain. Knee Surg Sports Traumatol Arthrosc 24(9):3011–3020
Franciozi CE, Ambra LF, Albertoni LJB, Debieux P, Granata GSM Jr, Kubota MS et al (2019) Anteromedial tibial tubercle osteotomy improves results of medial patellofemoral ligament reconstruction for recurrent patellar instability in patients with tibial tuberosity-trochlear groove distance of 17 to 20 mm. Arthroscopy 35(2):566–574
Franciozi CE, Ambra LF, Albertoni LJ, Debieux P, Rezende FC, Oliveira MA (2017) increased femoral anteversion influence over surgically treated recurrent patellar instability patients. Arthroscopy 33(3):633–640
Frosch KH, Schmeling A (2016) A new classification system of patellar instability and patellar maltracking. Arch Orthop Trauma Surg 136(4):485–497
Kaiser P, Schmoelz W, Schoettle P, Zwierzina M, Heinrichs C, Attal R (2017) Increased internal femoral torsion can be regarded as a risk factor for patellar instability: a biomechanical study. Clin Biomech (Bristol, Avon) 47(4):103–109
Kang H, Zheng R, Dai Y, Lu J, Wang F (2019) Single-and double-bundle medial patellofemoral ligament reconstruction procedures result in similar recurrent dislocation rates and improvements in knee function: a systematic review. Knee Surg Sports Traumatol Arthrosc 27(3):827–836
Kenawey M, Liodakis E, Krettek C, Ostermeier S, Horn T, Hankemeier S (2011) Effect of the lower limb rotational alignment on tibiofemoral contact pressure. Knee Surg Sports Traumatol Arthrosc 19(11):1851–1859
Keshmiri A, Maderbacher G, Baier C, Zeman F, Grifka J, Springorum HR (2016) Significant influence of rotational limb alignment parameters on patellar kinematics: an in vitro study. Knee Surg Sports Traumatol Arthrosc 24(8):2407–2414
Kita K, Tanaka Y, Toritsuka Y, Amano H, Uchida R, Takao R et al (2015) Factors affecting the outcomes of double-bundle medial patellofemoral ligament reconstruction for recurrent patellar dislocations evaluated by multivariate analysis. Am J Sports Med 43(12):2988–2996
Lee TQ, Anzel SH, Bennett KA, Pang D, Kim WC (1994) The influence of fixed rotational deformities of the femur on the patellofemoral contact pressures in human cadaver knees. Clin Orthop Relat Res 302(302):69–74
Longo UG, Vincenzo C, Mannering N, Ciuffreda M, Salvatore G, Berton A et al (2018) Trochleoplasty techniques provide good clinical results in patients with trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc 26(9):2640–2658
Mulliez A, Lambrecht D, Verbruggen D, Van Der Straeten C, Verdonk P, Victor J (2017) Clinical outcome in MPFL reconstruction with and without tuberositas transposition. Knee Surg Sports Traumatol Arthrosc 25(9):2708–2714
Nelitz M, Wehner T, Steiner M, Dürselen L, Lippacher S (2014) The effects of femoral external derotational osteotomy on frontal plane alignment. Knee Surg Sports Traumatol Arthrosc 22(11):2740–2746
Neri T, Parker DA, Beach A, Gensac C, Boyer B, Farizon F et al (2019) Medial patellofemoral ligament reconstruction with or without tibial tubercle transfer is an effective treatment for patellofemoral instability. Knee Surg Sports Traumatol Arthrosc 27(3):805–813
Nomura E, Horiuchi Y, Kihara M (2000) Medial patellofemoral ligament restraint in lateral patellar translation and reconstruction. Knee 7(2):121–127
Ntagiopoulos PG, Sharma B, Bignozzi S, Lopomo N, Colle F, Zaffagnini S, Dejour D (2013) Are the tubular grafts in the femoral tunnel in an anatomical or isometric position in the reconstruction of medial patellofemoral ligament? Int Orthop 37(10):1933–1941
Pal S, Draper CE, Fredericson M, Gold GE, Delp SL, Beaupre GS et al (2011) Patellar maltracking correlates with vastus medialis activation delay in patellofemoral pain patients. Am J Sports Med 39(3):590–598
Pal S, Besier TF, Beaupre GS, Fredericson M, Delp SL, Gold GE (2013) Patellar maltracking is prevalent among patellofemoral pain subjects with patella alta: an upright, weight bearing MRI study. J Orthop Res 31(3):448–457
Palmu S, Kallio PE, Donell ST, Helenius I, Nietosvaara Y (2008) Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Jt Surg Am 90:463–470
Peter G, Hoser C, Runer A, Abermann E, Wierer G, Fink C (2018) Medial patellofemoral ligament (MPFL) reconstruction using quadriceps tendon autograft provides good clinical, functional and patient-reported outcome measurements (PROM): a 2-year prospective study. Knee Surg Sports Traumatol Arthrosc 27(8):2426–2432
Post WR (1999) Clinical evaluation of patients with patellofemoral disorders. Arthroscopy 15(8):841–851
Roessler PP, Wimmer MD, Jacobs C, Bornemann R, Stein T, Lahner M (2018) Medial patellofemoral ligament reconstruction fails to correct mild patella alta in cases of patellofemoral instability-a case-control study. Int Orthop. https://doi.org/10.1007/s00264-018-4162-x
Rogers BA (2007) Patella alta: association with patellofemoral alignment and changes in contact area during weight-bearing. J Bone Jt Surg Am 90(2):1749–1755
Sappey-Marinier E, Sonnery-Cottet B, O'Loughlin P, Ouanezar H, Reina Fernandes L, Kouevidjin B et al (2019) Clinical outcomes and predictive factors for failure with isolated mpfl reconstruction for recurrent patellar Instability: a series of 211 reconstructions with a minimum follow-up of 3 years. Am J Sports Med 47(6):1323–1330
Schöttle PB, Schmeling A, Rosenstiel N, Weiler A (2007) Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med 35(5):801–804
Sheehan FT, Derasari A, Fine KM, Brindle TJ, Alter KE (2010) Q-angle and J-sign: indicative of maltracking subgroups in patellofemoral pain. Clin Orthop Relat Res 468(1):266–275
Souza RB, Draper CE, Fredericson M, Powers CM (2010) Femur rotation and patellofemoral joint kinematics: a weight-bearing magnetic resonance imaging analysis. J Orthop Sports Phys Ther 40(5):277–285
Takagi S, Sato T, Watanabe S, Tanifuji O, Mochizuki T, Omori G et al (2018) Alignment in the transverse plane, but not sagittal or coronal plane, affects the risk of recurrent patella dislocation. Knee Surg Sports Traumatol Arthrosc 26(10):2891–2898
Teng HL, Chen YJ, Powers CM (2014) Predictors of patellar alignment during weight bearing: An examination of patellar height and trochlear geometry. Knee 21(1):142–146
Van Haver A, De Roo K, De Beule M, Labey L, De Baets P, Dejour D et al (2015) The effect of trochlear dysplasia on patellofemoral biomechanics: a cadaveric study with simulated trochlear deformities. Am J Sports Med 43(6):1354–1361
Wagner D, Pfalzer F, Hingelbaum S, Huth J, Mauch F, Bauer G (2013) The influence of risk factors on clinical outcomes following anatomical medial patellofemoral ligament (MPFL) reconstruction using the gracilis tendon. Knee Surg Sports Traumatol Arthrosc 21(2):318–324
Xue Z, Song GY, Liu X, Zhang H, Wu G, Qian Y et al (2018) Excessive lateral patellar translation on axial computed tomography indicates positive patellar J-sign. Knee Surg Sports Traumatol Arthrosc 26(12):3620–3625
Yang Y, Zhang Q (2018) Reconstruction of the medial patellofemoral ligament and reinforcement of the medial patellotibial ligament is an effective treatment for patellofemoral instability with patella alta. Knee Surg Sports Traumatol Arthrosc 27(8):2599–2607
Zaffagnini S, Previtali D, Tamborini S, Pagliazzi G, Filardo G, Candrian C (2019) Recurrent patellar dislocations: trochleoplasty improves the results of medial patellofemoral ligament surgery only in severe trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05469-4
Funding
Funded by Beijing municipal administration of hospitals’ ascent plan (Grant No. DFL20180402).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no confict of interest.
Ethical approval
This study was approved by the ethics board of Beijing Jishuitan Hospital.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary file1 J-sign grade 1(.MP4). Female, 23, RPD for 5 years (right), J-sign (+), the lateral shift of patella during terminal knee extension was more than 1 quadrant of the patella (grade 1 J-sign) (MP4 555 kb)
Supplementary file2 J-sign grade 2(.MP4). Female, 18, RPD for 5 years (left), J-sign(+), the lateral shift of patella during terminal knee extension was more than 2 quadrants of patella (grade 2 J-sign) (MP4 416 kb)
Supplementary file3 J-sign grade 3 (grade 3 J-sign) (.MP4). Female, 32, RPD for 15 years (left), the patella dislocated completely in terminal knee extension and locked in subsequent flexion. The manual force was needed to unlock the patellofemoral joint. (MP4 1449 kb)
Rights and permissions
About this article
Cite this article
Zhang, Z., Zhang, H., Song, G. et al. A pre-operative grade 3 J-sign adversely affects short-term clinical outcome and is more likely to yield MPFL residual graft laxity in recurrent patellar dislocation. Knee Surg Sports Traumatol Arthrosc 28, 2147–2156 (2020). https://doi.org/10.1007/s00167-019-05736-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05736-4