Abstract
Purpose
To evaluate the knowledge and awareness of Evidence-Based Medicine (EBM) among members of the European Society of Sports Traumatology, Knee Surgery and Arthroscopy (ESSKA).
Methods
A questionnaire was developed that explored the following areas: (i) respondents’ attitudes to EBM; (ii) their motivation to implement EBM in daily practice; (iii) their educational background, knowledge and skills related to accessing and interpreting information; (iv) their level of attention to, and use of, scientific literature; (v) access to and availability of evidence; (vi) perceived barriers in using EBM in clinical practice. The resulting data were analyzed using descriptive statistics, and the correlation between age, educational background and country was further investigated.
Results
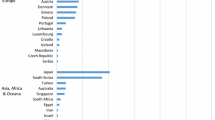
Two-hundred and eighty-eight ESSKA members (11% of the total population) compiled the questionnaire. The participants covered all the five continents and an expected prevalence of European professionals (77%) was observed. The vast majority of participants were medical doctors (91%), mainly specialized in knee surgery with minimal involvement in research. 97% of the participants declared having some knowledge of EBM, acquired mainly during their professional education, with some geographical differences. The youngest clinicians and those from Eastern Europe reported the greatest difficulty in using EBM in daily practice. The application of EBM in clinical practice is positively affected by the time dedicated to research and negatively correlates with the time dedicated to patient care.
Conclusions
The results of this survey highlight the need for further investigation into the main reasons behind the limited diffusion of the EBM approach, despite the medical community’s knowledge and interest in the concept. A wider application of EMB would upgrade clinical practice, linking medical knowledge and scientific evidence to patients’ needs which would result of benefit to patients, but also more in general to the health system.



Similar content being viewed by others
References
Ahmadi N, McKenzie ME, MacLean A, Brown CJ, Mastracci T, McLeod RS (2012) Teaching evidence based medicine to surgery residents-is journal club the best format? A systematic review of the literature. J Surg Educ 69:91–100
Artino AR, Durning SJ, Sklar DP (2018) Guidelines for reporting survey-based research submitted to academic medicine. Acad Med 93:337–340
Bennett S, Mckenna K, Hoffmann T, Tooth L, Mccluskey A, Strong J (2007) The value of an evidence database for occupational therapists: An international online survey. Int J Med Inf 76:507–513
Chalmers L (1983) Scientific inquiry and authoritarianism in perinatal care and education. Birth 10:151–166
Evidence-Based Medicine Working Group (1992) Evidence-based medicine. A new approach to teaching the practice of medicine. JAMA 268:2420–2425
Ganeshkumar P, Gopalakrishnan S (2013) Systematic reviews and meta-analysis: Understanding the best evidence in primary healthcare. J Fam Med Prim Care 2:9
Guyatt G (1992) Evidence-based medicine: a new approach to teaching the practice of medicine. JAMA 268:2420
Haynes B, Haines A (1998) Barriers and bridges to evidence based clinical practice. BMJ 317:273–276
Heiwe S, Kajermo KN, Tyni-Lenne R, Guidetti S, Samuelsson M, Andersson I-L, Wengstrom Y (2011) Evidence-based practice: attitudes, knowledge and behaviour among allied health care professionals. Int J Qual Health Care 23:198–209
Herbert R, Jamtvedt G, Hagen KB (2016) Practical evidence-based physiotherapy. Churchill Livingstone, London (2011 ProQuest Ebrary)
Hurwitz S (2003) Evidence-based medicine in orthopaedic surgery—a way to the future. Iowa Orthop J 23:61–65
Jette DU, Bacon K, Batty C, Carlson M, Ferland A, Hemingway RD, Hill JC, Ogilvie L, Volk D (2003) Evidence-based practice: beliefs, attitudes, knowledge, and behaviors of physical therapists. Phys Ther 83:786–805
MAGICapp https://magicproject.org/. Accessed 11 June 2019
Majid S, Foo S, Luyt B, Zhang X, Theng Y-L, Chang Y-K, Mokhtar IA (2011) Adopting evidence-based practice in clinical decision making: nurses’ perceptions, knowledge, and barriers. J Med Libr Assoc JMLA 99:229–236
Mallidi JR (2017) The challenges in practice of evidence based medicine. J Circ 1:2
Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS (1996) Evidence based medicine: what it is and what it isn’t. BMJ 312:71–72
Slowther A, Ford S, Schofield T (2004) Ethics of evidence based medicine in the primary care setting. J Med Ethics 30:151–155
Sung J, Siegel J, Tornetta P, Bhandari M (2008) The orthopaedic trauma literature: an evaluation of statistically significant findings in orthopaedic trauma randomized trials. BMC Musculoskelet Disord 9:14
Vogel EW (1999) Challenges to using evidence-based medicine in daily clinical practice. Semin Med Pract 2:21–24
Acknowledgements
The authors wish to thank Zhanna Kovalchuk, Executive Director, and Anna Hansen Rak, Office Manager, of ESSKA a.s.b.l., Luxembourg, for their support with the survey circulation; Davide Corbetta and Riccardo Negri for their help and assistance with the pilot study.
Funding
The project was funded by the Italian Ministry of Health, Ricerca Corrente, Progetto “Revisioni sistematiche della letteratura scientifica in ortopedia, traumatologia e riabilitazione funzionale”.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lugano, G., Gianola, S., Castellini, G. et al. Evidence-Based Medicine (EBM) is properly perceived but its application is still limited in the orthopedic clinical practice: an online survey among the European Society of Sports Traumatology, Knee Surgery and Arthroscopy (ESSKA) members. Knee Surg Sports Traumatol Arthrosc 28, 1665–1672 (2020). https://doi.org/10.1007/s00167-019-05670-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05670-5