Abstract
Purpose
Both coronal and sagittal laxity of well-functioning knees after total knee arthroplasty (TKA) was examined, and the correlations between the joint laxity and the clinical outcomes were analyzed to clarify the adequate joint laxity for the prosthesis, and the relationship between the laxity and the outcomes.
Methods
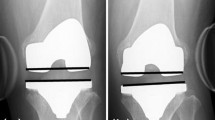
Forty well-functioning TKA knees with a high-flexion posterior-stabilized (PS) prosthesis were studied. All patients were diagnosed as having osteoarthritis with varus deformity and were followed up for 2 years or more. The coronal and sagittal laxity was assessed at extension and flexion, and the correlations between the joint laxity and the clinical outcomes were evaluated.
Results
The varus and valgus laxity averaged 5.6 ± 1.8° and 3.6 ± 1.2° at 10° knee flexion, and 7.4 ± 5.1° and 3.6 ± 2.7° at 80° knee flexion, respectively, and the AP laxity at 30° and 75° knee flexion averaged 8.7 ± 3.6 mm and 6.6 ± 2.3 mm, respectively. Knee flexion angle correlated with the joint laxity, while the other outcomes including patient-reported pain and instability were adversely affected by the greater laxity.
Conclusions
This study exhibited the importance of consistent medial laxity both at extension and flexion, which averaged 3.6°. Care should be taken to maintain the medial stability and to obtain adequate laxity both at extension and flexion during surgery. A few degrees of medial tightness can be allowed to achieve excellent clinical results after TKA for preoperative varus knees.
Level of evidence
Therapeutic study, Level III.




Similar content being viewed by others
Change history
28 May 2019
Unfortunately, the co-author “Hiroki Katagiri’ was omitted in the original publication from the author group. The author name is added here. The original article has been corrected.
References
Bourne RB, Chesworth B, Davis A, Mahomed N, Charron K (2010) Comparing patient outcomes after THA and TsKA: is there a difference? Clin Orthop Relat Res 468:542–546
Calliess T, Ettinger M, Hulsmann N, Ostermeier S, Windhagen H (2015) Update on the etiology of revision TKA—evident trends in a retrospective survey of 1449 cases. Knee 22:174–179
Dejour D, Deschamps G, Garotta L, Dejour H (1999) Laxity in posterior cruciate sparing and posterior stabilized total knee prostheses. Clin Orthop Relat Res 364:182–193
Hino K, Kutsuna T, Watamori K, Kiyomatsu H, Ishimaru Y, Takeba J et al (2017) Varus-valgus stability at 90 degrees flexion correlates with the stability at midflexion range more widely than that at 0 degrees extension in posterior-stabilized total knee arthroplasty. Arch Orthop Trauma Surg 137:1429–1434
Ishii Y, Noguchi H, Takeda M, Sato J, Sakurai T, Toyabe S (2014) In vivo anteroposterior translation after meniscal-bearing total knee arthroplasty: effects of soft tissue conditions and flexion angle. Eur J Orthop Surg Traumatol 24:967–971
Jones DP, Locke C, Pennington J, Theis JC (2006) The effect of sagittal laxity on function after posterior cruciate-retaining total knee replacement. J Arthroplast 21:719–723
Kamenaga T, Muratsu H, Kanda Y, Miya H, Kuroda R, Matsumoto T (2018) The influence of postoperative knee stability on patient satisfaction in cruciate-retaining total knee arthroplasty. J Arthroplasty 33:2475–2479
Kuster MS, Bitschnau B, Votruba T (2004) Influence of collateral ligament laxity on patient satisfaction after total knee arthroplasty: a comparative bilateral study. Arch Orthop Trauma Surg 124:415–417
Matsuda Y, Ishii Y, Noguchi H, Ishii R (2005) Varus-valgus balance and range of movement after total knee arthroplasty. J Bone Jt Surg Br 87:804–808
Matsumoto K, Ogawa H, Yoshioka H, Akiyama H (2017) Postoperative anteroposterior laxity influences subjective outcome after total knee arthroplasty. J Arthroplasty 32:1845–1849
Nabeyama R, Matsuda S, Miura H, Kawano T, Nagamine R, Mawatari T et al (2003) Changes in anteroposterior stability following total knee arthroplasty. J Orthop Sci 8:526–531
Nakahara H, Okazaki K, Hamai S, Okamoto S, Kuwashima U, Higaki H et al (2015) Does knee stability in the coronal plane in extension affect function and outcome after total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc 23:1693–1698
Okamoto S, Okazaki K, Mitsuyasu H, Matsuda S, Mizu-Uchi H, Hamai S et al (2014) Extension gap needs more than 1-mm laxity after implantation to avoid post-operative flexion contracture in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22:3174–3180
Okazaki K, Miura H, Matsuda S, Takeuchi N, Mawatari T, Hashizume M et al (2006) Asymmetry of mediolateral laxity of the normal knee. J Orthop Sci 11:264–266
Petrie JR, Haidukewych GJ (2016) Instability in total knee arthroplasty: assessment and solutions. Bone Jt J 98-B:116–119
Scuderi GR, Deshmane PP (2015) Instability of total knee replacement. In: Hirschmann MT, Becker R (eds) The unhappy total knee replacement. Springer, New York, pp 195–205
Seah RB, Yeo SJ, Chin PL, Yew AK, Chong HC, Lo NN (2014) Evaluation of medial-lateral stability and functional outcome following total knee arthroplasty: results of a single hospital joint registry. J Arthroplasty 29:2276–2279
Tsukiyama H, Kuriyama S, Kobayashi M, Nakamura S, Furu M, Ito H et al (2017) Medial rather than lateral knee instability correlates with inferior patient satisfaction and knee function after total knee arthroplasty. Knee 24:1478–1484
Watanabe T, Muneta T, Koga H, Horie M, Nakamura T, Otabe K et al (2016) In-vivo kinematics of high-flex posterior-stabilized total knee prosthesis designed for Asian populations. Int Orthop 40:2295–2302
Watanabe T, Muneta T, Sekiya I, Banks SA (2013) Intraoperative joint gaps affect postoperative range of motion in TKAs with posterior-stabilized prostheses. Clin Orthop Relat Res 471:1326–1333
Watanabe T, Muneta T, Yagishita K, Hara K, Koga H, Sekiya I (2016) Closed suction drainage is not necessary for total knee arthroplasty: a prospective study on simultaneous bilateral surgeries of a mean follow-up of 5.5 years. J Arthroplasty 31:641–645
Wautier D, Thienpont E (2017) Changes in anteroposterior stability and proprioception after different types of knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25:1792–1800
Yamakado K, Kitaoka K, Yamada H, Hashiba K, Nakamura R, Tomita K (2003) Influence of stability on range of motion after cruciate-retaining TKA. Arch Orthop Trauma Surg 123:1–4
Yoshihara Y, Arai Y, Nakagawa S, Inoue H, Ueshima K, Fujiwara H et al (2015) Assessing coronal laxity in extension and flexion at a minimum of 10 years after primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24:2512–2516
Funding
No external source of funding was used.
Author information
Authors and Affiliations
Contributions
TW created the study design, conducted the study, collected, analyzed and interpreted the data, drafted the manuscript and completed the final manuscript. HKo, HKa, KO, YN, TM, IS and TJ conducted the study, collected the data and revised the drafted manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the institutional review board of the Tokyo Medical and Dental University.
Informed consent
Written informed consent was obtained from all participants included in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: The co-author “Hiroki Katagiri” was omitted in the original publication and updated here.
Rights and permissions
About this article
Cite this article
Watanabe, T., Koga, H., Katagiri, H. et al. Coronal and sagittal laxity affects clinical outcomes in posterior-stabilized total knee arthroplasty: assessment of well-functioning knees. Knee Surg Sports Traumatol Arthrosc 28, 1400–1409 (2020). https://doi.org/10.1007/s00167-019-05500-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05500-8